|
Case Report
A rare case, severe preeclampsia in pregnancy with massive mucin ovarium cyst: A case report
1 Obstetrics and Gynecology Department, Hasanuddin University, Makassar 90245, Indonesia
2 Wahidin Sudirohusodo General Hospital, Makassar 90245, Indonesia
Address correspondence to:
Deviana Soraya Riu
Obstetrics and Gynecology Department, Hasanuddin University, Makassar 90245,
Indonesia
Message to Corresponding Author
Article ID: 100087Z08DR2021
Access full text article on other devices
Access PDF of article on other devices

How to cite this article
Riu DS, Lukas E, Wewengkang ET. A rare case, severe preeclampsia in pregnancy with massive mucin ovarium cyst: A case report. J Case Rep Images Obstet Gynecol 2021;7:100087Z08DR2021.ABSTRACT
Preeclampsia is a disorder in pregnancy associated with hypertension, which occurs after 20 weeks of gestation. Mucin ovarian adenoma cysts are rare in adolescence and during pregnancy. A 30-year-old female G4P2A1 patient with severe preeclampsia accompanied by cystic ovarian neoplasms came to the emergency room with an active phase of labor at 32 weeks of gestation, breech presentation, and severe anemia. Blood transfusion, cesarean section, and left salpingo-oophorectomy were performed. The patient‘s blood pressure returned to normal after two months post-surgery. There is no causative evidence between severe preeclampsia and neoplasm events. It needs optimal supervision in pregnant patients accompanied by gynecological disorders because it has a high risk for a complication such as preeclampsia.
Keywords: Mucin ovarian cysts, Preterm, Severe preeclampsia
Introduction
Preeclampsia is a disorder in pregnancy associated with hypertension, which occurs after a gestational age of more than 20 weeks and often approaches term gestation [1]. Preeclampsia is estimated to be a complication in 2–8% of global pregnancy rates [1]. Complications of malignancy in pregnancy are 1 in 1000 pregnancies, and the prevalence is higher in the benign neoplasm [2]. Ovarian mucinous cystadenoma is a benign tumor originating from the epithelial surface of the ovary. These cysts are multilocular with a smooth outer and inner surface and tend to grow enormously [3],[4] The percentage of mucin ovarian cysts is 15–20% of all existing ovarian tumors, and only 10% are borderline type [5],[6]. This mucin ovarian adenoma cyst rarely occurs during adolescence and pregnancy [7]. One-third of borderline mucinous tumors are diagnosed in women before 40 years old, the epidemiology and management of this tumors during pregnancy also still little known [8]. Borderline mucinous tumor mostly diagnosed during the first trimester and found it incidentally [9].
Case Report
Patient information
This paper reports a 30-year-old woman, G4P2A1, diagnosed with cystic ovarian neoplasm two years ago and was advised to do surgery, but the patient refused. The patient did not realize that she was pregnant because she had irregular menstrual cycles and an enlarged abdomen due to the tumor. Pregnancy was diagnosed at 28 weeks gestational age when the patient decided to do surgery because she felt the tumor was getting bigger. At that time the patient diagnosed with hypertension also. Pregnancy termination at 32 weeks of gestation because of signs of labor, accompanied by symptoms of severe preeclampsia and severe anemia with breech presentation. The patient was given a two-bag packed red cell (PRC) transfusion, emergency cesarean section, and followed by a left salpingo-oophorectomy.
Clinical findings
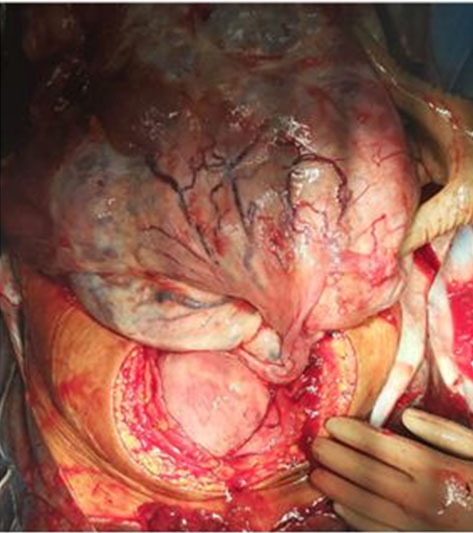
The patient had a blood pressure of 170/100 mmHg with positive proteinuria 1 (+), hypertension diagnosed since 28 weeks of gestation. On Leopold’s examination, uterine fundal height cannot be assessed because the tumor mass covered it. On vaginal examination, it was found that the cervix dilated 7 cm, with a small part of the fetus (legs) was felt. On transabdominal ultrasound examination, it was found that multilocus cysts filled the entire monitor screen without any solid mass images (Figure 1). The patient appeared pale, conjunctival anemic with a hemoglobin value of 5.7 g/dL. Intraoperatively we found the left ovarian size was approximately 35 × 40 cm on abdominal cavity and for the right ovarian one was 3 × 3 cm in size, oval in shape, lie on the posterior wall of the pelvis, lateral to the uterus (Figure 2).
The course of disease
Diagnostic assessment
The results of the anatomic pathology examination of ovarian tissue concluded that borderline mucinous ovarian tumors and cytology results from ascitic fluid did not show the presence of malignant epithelial cells. Hemoglobin level post-transfusion PRC even bag was 11 g/dL, tumor marker was Ca-125: 84.19 U/mL, and proteinuria + (positive-1).
Treatment intervention and follow-up
The patient received an MgSO4 intravenous and a two-bag PRC transfusion. Cesarean section was performed with a midline incision, and a baby boy was born; birth weight was 1900 grams, length 40 cm, Apgar scores 6/9. The ovarian tumor was identified. Adhesion looks between the tumor with the intestine and the omentum. Adhesiolysis performed first and then a left salpingo-oophorectomy. On day five, post-operation, the patient’s blood pressure was still unstable with a value of 184/123 mmHg. The patient consulted the Nephrology and Hypertension division and received combination therapy of Amlodipine 10 mg/8 hours/oral and Captopril 12.5 mg/8 hours/oral, which continued until two months post-surgery. The patient’s blood pressure is within normal limits and free from antihypertensive medication already.
Discussion
A study states that preeclampsia is associated with a 1.23-fold increased risk of developing cancer in all organs and even more than two times the risk of ovarian cancer. However, a report states that preeclampsia has a protective effect for the occurrence of neoplasms in mothers with a history of preeclampsia who gave birth to a baby boy [10]. The patient was diagnosed with severe preeclampsia at 28 weeks of gestation, but she did not take medication regularly. Pregnancies accompanied by benign neoplasm have an increased risk of preterm delivery by 38% and tend to develop anemia [11],[12]. This patient has a low hemoglobin level, is classified as severe anemia, and the baby is born in preterm gestation. This mucinous type ovarian tumor often has an enormous size. A large tumor can cause complications due to compression effects, like tightness, pain, bloating, and urinary tract symptoms [7]. Preterm delivery at this patient due to the distension caused by the tumor initiates gap-junction protein, increasing maternal corticotropin-releasing hormone and estrogen levels, affecting myometrial contractility and cervical ripening [13]. Recurrence after cystectomy was 15% and one study recommended to do unilateral oophorectomy for conservative treatment because of the high recurrence after cystectomy [14]. There is no established guidelines for the best timing for the operation procedure, several groups suggest that the surgery to be performed between 14 and 22 weeks of gestation [8]. Conservative management is one of the good options also for women with borderline ovarian tumor who want to preserve their fertility [9].
The incidence of breech presentation is 10–15%, which in these patients is due to a tumor in the pelvis [15]. The mucin cyst on the left ovary with a large size causes the fetus to be pressed and unable to undergo intrauterine rotation so that the leg becomes the lowest part of the fetus. The best treatment for the mucinous type ovarian tumor is unilateral salpingo-oophorectomy or ovarian cystectomy [16]. This patient also underwent left salpingo-oophorectomy after the cesarean section.
Pregnant women with benign neoplasms increase the risk of gestational diabetes and preeclampsia and have a hospitalization period of approximately seven days or more or may experience rehospitalization [2]. This patient was treated for eight days, and after postoperative observation, the patient’s blood pressure had decreased, and the blood pressure returned to normal after routine treatment for two months.
In this case, the tumor that occurred was a unilateral tumor on the left ovary with a large size and filled with fluid with a thick and spongy consistency characteristic of mucinous ovarian tumors. After surgery, patients should be followed up regularly to anticipate recurrences [17],[18]. Even though this tumor was removed entirely, this patient was still scheduled for follow-up every three months for one year.
Approval
The patient acknowledges and agrees to the discussion and publication of the clinical condition she has experienced.
Conclusion
No evidence states a causative effect between preeclampsia and the incidence of neoplasms, and vice versa. It is necessary to closely monitor the mother and fetus in pregnant patients with neoplasm abnormalities, especially in high-risk patients, such as preeclampsia. In patients of reproductive age and known to have a neoplasm, counseling should be given to the use of contraceptives.
REFERENCES
1.
ACOG Practice Bulletin No. 202 Summary: Gestational hypertension and preeclampsia. Obstet Gynecol 2019;133(1):1. [CrossRef]
[Pubmed]

2.
Niu X, Li CI, Mueller BA. Obstetrical and infant outcomes among women with neoplasms during pregnancy. Cancer Causes Control 2019;30(6):651–61. [CrossRef]
[Pubmed]

3.
Mittal S, Gupta N, Sharma AK, Dadhwal V. Laparoscopic management of a large recurrent benign mucinous cystadenoma of the ovary. Arch Gynecol Obstet 2008;277(4):379–80. [CrossRef]
[Pubmed]

4.
Vizza E, Galati GM, Corrado G, Atlante M, Infante C, Sbiroli C. Voluminous mucinous cystadenoma of the ovary in a 13-year-old girl. J Pediatr Adolesc Gynecol 2005;18(6):419–22. [CrossRef]
[Pubmed]

5.
Gwanzura C, Muyotcha AF, Magwali T, Chirenje ZM, Madziyire MG. Giant mucinous cystadenoma: A case report. J Med Case Rep 2019;13(1):181. [CrossRef]
[Pubmed]

6.
Kamel RM. A massive ovarian mucinous cystadenoma: A case report. Reprod Biol Endocrinol 2010;8:24. [CrossRef]
[Pubmed]

7.
Somagutta MR, Luvsannyam E, Jain MS, et al. A rare case of massive ovarian mucinous cystadenoma with postmenopausal bleeding. Cureus 2020;12(9):e10198. [CrossRef]
[Pubmed]

8.
Casanova J, Maciel R, Ferreira V, Fernandes E, Rodrigues RM. Borderline ovarian tumor during pregnancy: A case report. Case Rep Obstet Gynecol 2013;2013:160319. [CrossRef]
[Pubmed]

9.
Fauvet, R, Brzakowski M, Morice P, et al. Borderline ovarian tumors diagnosed during pregnancy exhibit a high incidence of aggressive features: Results of a French multicenter study. Ann Oncol 2012;23(6):1481–7. [CrossRef]
[Pubmed]

10.
Calderon-Margalit R, Friedlander Y, Yanetz R, et al. Preeclampsia and subsequent risk of cancer: Update from the Jerusalem Perinatal Study. Am J Obstet Gynecol 2009;200(1):63.e1–5. [CrossRef]
[Pubmed]

11.
Coronado GD, Marshall LM, Schwartz SM. Complications in pregnancy, labor, and delivery with uterine leiomyomas: A population-based study. Obstet Gynecol 2000;95(5):764–9. [CrossRef]
[Pubmed]

12.
Haider BA, Olofin I, Wang M, et al. Anemia, prenatal iron use, and risk of adverse pregnancy outcomes: Systematic review and meta-analysis. BMJ 2013;346:f3443. [CrossRef]
[Pubmed]

13.
14.
Cosentino F, Turco LC, Cianci S, et al. Management, prognosis and reproductive outcomes of borderline ovarian tumor relapse during pregnancy: From diagnosis to potential treatment options. J Prenat Med 2016;10(1–2):8–14. [CrossRef]
[Pubmed]

15.
16.
Limaiem F, Lekkala MR, Mlika M. Ovarian Cystadenoma. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2021.
[Pubmed]

17.
18.
Fauvet R, Poncelet C, Boccara J, Descamps P, Fondrinier E, Daraï E. Fertility after conservative treatment for borderline ovarian tumors: A French multicenter study. Fertil Steril 2005;83(2):284–90. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Deviana Soraya Riu - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Efendi Lukas - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ellen T Wewengkang - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Deviana Soraya Riu et al.. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.