|
Case Series
Magnetic resonance imaging of non-communicating rudimentary horn with pregnancy and placenta accreta in a unicornuate uterus
1 Radiology Resident, Department of Medical Imaging, Rambam Health Care Campus, Haifa, Israel
2 Staff Radiologist, Rambam Health Care Campus, Haifa, Israel
3 Obstetrics and Gynecology Resident, Rambam Health Care Campus, Haifa, Israel
4 Head of the Division of Gynecologic-Oncology, Rambam Health Care Campus, Haifa, Israel
5 Director of Maternal-Fetal Medicine Service, Rambam Health Care Campus, Haifa, Israel
6 Chairman of Medical Imaging, Rambam Health Care Campus, HaAliya HaShniya St 8, Haifa, Israel
Address correspondence to:
Marcia C Javitt
MD, Director of Medical Imaging, Rambam Health Care Campus, Haifa 310961, Israel; Adjunct Professor of Radiology, The George Washington University School of Medicine, 2300 I St NW, Washington, DC 20052, USA; Chairman of Medical Imaging, Rambam Health Care Campus, HaAliya HaShniya St 8, Haifa 3109601,
Israel
Message to Corresponding Author
Article ID: 100088Z08BS2021
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Sokolovski B, Abadi S, David CB, Amit A, Solt I, Javitt MC. Magnetic resonance imaging of non-communicating rudimentary horn with pregnancy and placenta accreta in a unicornuate uterus. J Case Rep Images Obstet Gynecol 2021;7:100088Z08BS2021.ABSTRACT
Introduction: Mullerian anomalies are associated with an increased incidence of obstetrical complications including fetal demise. One such anomaly that can have dire consequences for both the pregnant mother and the fetus is the unicornuate uterus with a gravid noncommunicating rudimentary horn.
Case Series: Prompt diagnosis is critically important but often challenging using ultrasonography (US). Magnetic resonance imaging (MRI) can be decisive for accurate diagnosis, timely management, and optimization of outcome, especially in cases in which US is indeterminate. The first case demonstrates the relevant anatomy in a 12-year-old non-gravid female who presented with right lower quadrant pain. MRI showed a normal appendix and enabled identification of the congenital uterine anomaly. In the second case, MRI accurately showed a gravid noncommunicating rudimentary horn at 28 weeks gestation as well as four placental units with placenta accreta.
Conclusion: MRI can be essential in the diagnosis of and treatment planning for a unicornuate uterus with a gravid non-communicating rudimentary horn.
Keywords: MRI, Placenta accreta, Rudimentary horn pregnancy, Unicornuate uterus
Introduction
Embryology
The uterus normally develops from a pair of paramesonephric (i.e., Mullerian) ducts. These ducts fuse together after which the remaining midline structures are resorbed thereby forming the uterus. The most superior aspects of the two Mullerian ducts form the fallopian tubes that remain open to the peritoneal cavity. The inferior parts create the cervix and the upper third of the vagina. The lower two-thirds of the vagina develop from the sinovaginal bulbs that are in turn derived from the urogenital sinus. As the ovaries arise from the gonadal ridge, and not from the Mullerian ducts, Mullerian fusion anomalies generally do not affect the ovaries. Because paramesonephric ducts are involved in development of both renal and gynecologic structures, renal anomalies are often associated with Mullerian anomalies [1],[2],[3],[4].
The American Fertility Society (now referred to as the American Society for Reproductive Medicine) classification of uterine anomalies is based upon the embryologic and pathologic development of the Mullerian ducts. The class 1 anomaly is agenesis or hypoplasia of the uterus. Unicornuate uterus is a class 2 anomaly, caused by dysfunction of the paramesonephric ducts. Classes 3 and 4 are fusion defects resulting in didelphys uteri or bicornuate uteri, respectively. Classes 5 and 6 result from failure of septal resorption causing a spectrum of findings from arcuate to septate uteri [4],[5],[6].
Epidemiology
The reported prevalence of uterine anomalies [3] ranges from 1.9% on hysterosalpingography to 5.5% using three-dimensional ultrasound (3D US) performed in the general population on normal multiparous women [3],[7],[8],[9]. Septate uterus is the most common anomaly, followed by the bicornuate uterus [3],[10]. The prevalence of the unicornuate uterus has been reported as 5–9% of all Mullerian anomalies [11],[12]. According to the American Fertility Society classification system, there are four subtypes of the unicornuate uterus (Class 2 anomalies are shown in Table 1).
The reported prevalence for subtypes of unicornuate uteri are as follows: Class 2A—10%, Class 2B—22%, Class 2C—33%, and Class 2D—35% [3],[13]. A more recent study reported that the prevalence of Class 2C was 48%, and of Class 2B was 38% [12].
Pregnancy in a rudimentary horn is an extremely rare condition with an estimated incidence between one in 76,000 to one in 140,000 pregnancies [14],[15]. 33% of rudimentary horns are non-cavitary, 22% are cavitary but non-communicating, and 10% are cavitary and communicating [3],[16]. When the rudimentary horn is cavitary but non-communicating with the main uterine body, a rudimentary horn pregnancy can lead to uterine rupture that threatens survival of both mother and child.
Fertilization of gestations occurring in non-communicating cavitary rudimentary uterine horns is thought to occur via transperitoneal migration of sperm or possibly of fertilized ova [17],[18]. Although such pregnancies are rare, they have the highest risk of fetal death of all congenital uterine malformations [19].
Presentation and complications
Unicornuate uterus with a cavitary rudimentary horn has both gynecologic and obstetric complications including infertility, endometriosis and adenomyosis, hematometra, urinary tract anomalies, ectopic pregnancies, recurrent abortions, preterm labor and deliveries, fetal death, intrauterine growth retardation, fetal malpresentation, a higher rate of caesarean sections, and incompetent cervix [18][20],[21],[22].
The prognosis for a pregnancy in a non-communicating rudimentary horn is poor. The incidence of uterine rupture is 90%. Rupture usually occurs in the second trimester, with only 2% fetal survival. Indeed, patients often present in extremis with hypotension or shock and hemoperitoneum from bleeding that threatens the survival of both mother and fetus [19],[23].
The most commonly associated renal anomaly with unicornuate uterus is renal agenesis, though ectopic kidney, horseshoe kidneys, and incompletely rotated kidneys have been reported [20],[22]. Patients with renal agenesis are especially prone to pregnancy-induced hypertension and proteinuria [22].
Placenta accreta with a rudimentary horn pregnancy was first reported by Heinonen [18]. Because placenta accreta has an abnormal placental attachment to the myometrium, it generally has a major risk of bleeding during delivery and post-partum [24]. Oral et al. estimated the incidence of placenta accreta in rudimentary horn pregnancies at about 11.9%, indicating that this complication is more common with rudimentary than intrauterine pregnancies [25].
Imaging
The diagnosis of a rudimentary uterine horn with a unicornuate uterus is challenging. Hysterosalpingography (HSG), typically performed for evaluation of tubal patency in infertility, demonstrates only the contralateral patent cavity in the main uterine body without visualization of the non-communicating rudimentary horn [3],[26]. Ultrasonography (US) has a major role in the early diagnosis of rudimentary horn pregnancy, especially in early gestation [26],[27],[28]. Three-dimensional ultrasound (3D US) demonstrates the anatomy to advantage in the first trimester as the entire uterine duplication may be included in a single imaged volume [29] but this modality becomes more limited with advancing gestational age as the uterus enlarges, extends above the pelvic brim, and imaging can be obscured by bowel gas.
The sonographic differential diagnosis includes tubal pregnancy, interstitial ectopic pregnancy, abdominal pregnancy, and pregnancy in a bicornuate uterus. The circumferential surrounding myometrium in the rudimentary horn distinguishes it from a tubal ectopic pregnancy. The clear margin of placenta can differentiate it from an abdominal pregnancy, and variable myometrial thickness with greater distance between the uterine horns can be diagnostic for unicornuate uterus’s rudimentary horn as opposed to a gravid bicornuate uterus [28],[30]. There is no connection between the pregnant unicornuate horn and the single cervical canal, which is in continuity only with the endometrial canal of the main uterine body [30]. Other diagnostic criteria for rudimentary horn pregnancy have been suggested: (1) a single interstitial portion of fallopian tube in the main uterine body, (2) a mobile and separate gestational sac surrounded by myometrium, and (3) a vascular pedicle between the gestational sac and unicornuate uterus [31].
Despite these detailed diagnostic criteria, the estimated sensitivity of US for diagnosis of a rudimentary horn in general is limited [3], with low sensitivity reported between 26% [27] to 33.3% [14] for the sonographic diagnosis of rudimentary horn pregnancies before rupture.
3D US has been used in the characterization of Mullerian anomalies with the advantages of safety (i.e., without ionizing radiation) and wide accessibility. 3D US depicts of the fundal contour of the uterus to advantage, similar to MRI [32]. With both high sensitivity and specificity for Mullerian anomalies [32],[33], 3D US has been used successfully for diagnosis of a rudimentary horn pregnancy [34]. Although it is usually concordant with MRI for fundal contour, 3D US is less accurate than MRI for studying the remainder of the uterus [33]. Moreover, the non-cavitary rudimentary horn may be overlooked on US [20]. MRI, the gold standard in diagnosing Mullerian anomalies, is used for problem solving after inconclusive US [4].
MRI shows the lenticular shape with reduced volume, asymmetric uterine configuration, and presence or absence of endometrial lining in the rudimentary horn. The presence of central high T2 signal intensity in a rudimentary horn indicates a cavitary rudimentary horn (i.e., lined by endometrium) [3],[35]. Magnetic resonance imaging may provide better information about the endometrial-myometrial ratio that correlates with congenital uterine anomalies and infertility [3],[35],[36]than hysteroscopy and laparoscopy combined.
The following cases illustrate the important MR diagnostic criteria, some associated complications, and challenging management of this condition.
Reprinted with permission from Elsevier from Table 5 in The American Fertility Society classifications of adnexal adhesions, distal tubal occlusion, tubal occlusion secondary to tubal ligation, tubal pregnancies, Mullerian anomalies and intrauterine adhesions. Fertil Steril, 1988; 49:944–955.
CASE SERIES
Case 1—The appearance in a non-gravid uterus
A 12-year-old female presented with severe right lower quadrant abdominal pain at menarche. She had pallor, normal vital signs, and tenderness in the right lower quadrant. She had no fever or leukocytosis. Hemoglobin was 11.9 g/dL.
The appendix was normal on transabdominal US, but there was a tubular hypoechoic structure measuring 7.5 cm L × 5.5 cm AP × 4.0 cm W with low level internal echoes and absent color flow on Doppler interrogation. The right ovary was not sonographically identified. Diagnostic laparoscopy performed due to clinical suspicion of right ovarian torsion revealed a right hematosalpinx arising from a non-communicating right rudimentary horn in a unicornuate uterus and normal ovaries. Subsequent hysteroscopy showed a single cervix leading to the main left uterine horn.
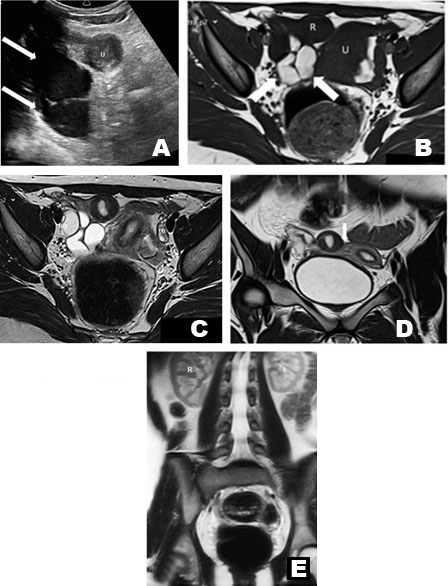
Pelvic MRI performed one month later confirmed the non-communicating right cavitary horn, the main left horn with a normal cervix, and a right hematosalpinx showing bright signal intensity with dependent low T2 signal representing retracted clot. The ovaries were normal (Figure 1). The patient underwent an elective right hemi-hysterectomy with ipsilateral salpingectomy.
Case 2—Gravid non-communicating rudimentary horn with placenta accreta spectrum
A 34–year-old G2P1A2 pregnant female at 27 weeks estimated gestational age both by dates and projected from a first trimester US was referred for suspected polyhydramnios, severe intrauterine growth retardation, and absent end-diastolic flow on fetal umbilical artery Doppler on outside US. Physical examination revealed a single cervix.
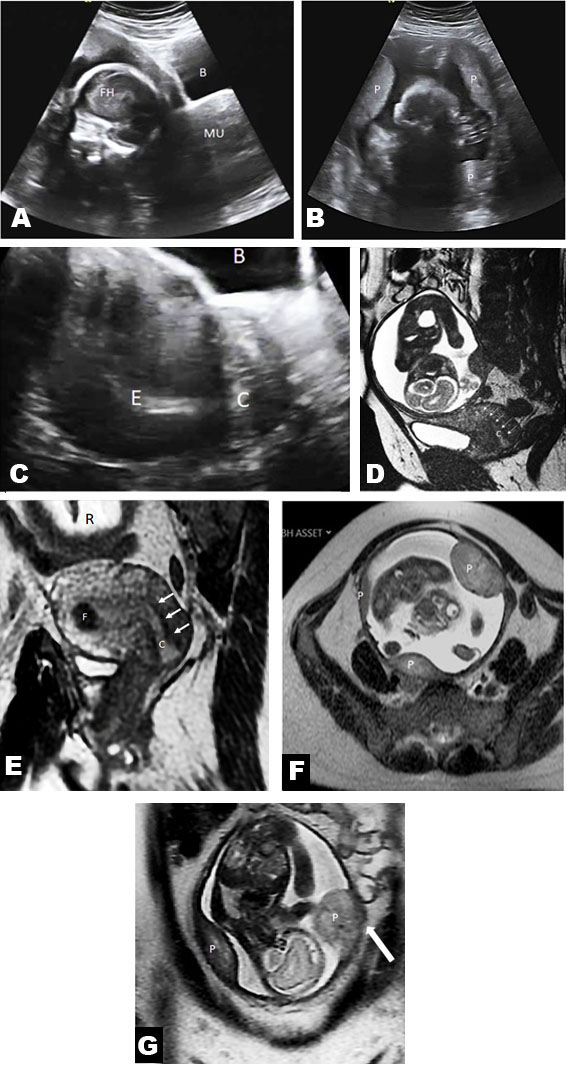
A gravid uterus and a single cervix were identified on physical examination. Repeat US showed an empty left uterine horn with normal cervix, and a separate pregnancy of uncertain anatomic location in the right pelvis. An MRI was requested to clarify whether there was an abdominal or other ectopic pregnancy, or a uterine anomaly. Magnetic resonance imaging on a 1.5 Tesla superconducting magnet revealed an empty left unicornuate uterus with a single cervix. The right rudimentary horn contained a 25-week live gestation. There were 4 separate placental lobes with multifocal abnormally invasive placenta (both placenta increta and percreta). No polyhydramnios was seen. The maternal kidneys were normotopic (Figure 2).
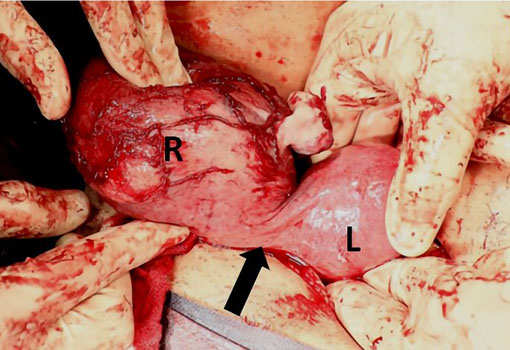
These findings were presented to the patient emphasizing the complexity of and risk for maintaining such pregnancy, including risk of uterine rupture, and the unfavorable prognosis of the fetus. The patient requested termination of the pregnancy. After approval of the patient’s request by the hospital’s pregnancy termination committee, feticide was performed by potassium chloride injection [10 mmol/L (0.75 g) in 10 mL] into the fetal heart with sonographic guidance. The patient underwent a right hemi-hysterectomy and right salpingectomy (Figure 3). Severe intrauterine growth retardation that was diagnosed by ultrasound prenatally was confirmed at surgery. One year later, the patient became pregnant within the main uterine horn, now entering her third trimester of that pregnancy uneventfully at the time of this writing.
Discussion
An algorithmic approach to MRI interpretation of Mullerian duct anomalies was introduced by Robbins et al. [4]. Although various publications discussed the MRI diagnosis of an empty rudimentary horn [3],[4],[35],[36], there are only a few reports that describe the MRI findings in a gravid non-communicating rudimentary horn [30],[37]. The superiority of MRI for diagnosis of a unicornuate uterus with pregnancy in a non-communicating rudimentary horn is exemplified by Case 2. The dire consequences of uterine rupture and coexisting placenta accreta spectrum were avoided.
Conclusion
We recommend the use of MRI for problem solving after indeterminate US and for clarification of the many known complications for a unicornuate uterus with pregnancy in a non-communicating rudimentary horn.
REFERENCES
1.
2.
Crosby WM, Hill EC. Embryology of the Mullerian duct system. Review of present-day theory. Obstet Gynecol 1962;20:507–5.
[Pubmed]

3.
Troiano RN, McCarthy SM. Mullerian duct anomalies: Imaging and clinical issues. Radiology 2004;233(1):19–34. [CrossRef]
[Pubmed]

4.
Robbins JB, Broadwell C, Chow LC, Parry JP, Sadowski EA. Müllerian duct anomalies: Embryological development, classification, and MRI assessment. J Magn Reson Imaging 2015;41(1):1-12. [CrossRef]
[Pubmed]

5.
The American Fertility Society classifications of adnexal adhesions, distal tubal occlusion, tubal occlusion secondary to tubal ligation, tubal pregnancies, Müllerian anomalies and intrauterine adhesions. Fertil Steril 1988;49(6):944–55. [CrossRef]
[Pubmed]

6.
7.
Ashton D, Amin HK, Richart RM, Neuwirth RS. The incidence of asymptomatic uterine anomalies in women undergoing transcervical tubal sterilization. Obstet Gynecol 1988;72(1):28–30.
[Pubmed]

8.
Jurkovic D, Gruboeck K, Tailor A, Nicolaides KH. Ultrasound screening for congenital uterine anomalies. Br J Obstet Gynaecol 1997;104(11):1320–1. [CrossRef]
[Pubmed]

9.
Chan YY, Jayaprakasan K, Zamora J, Thornton JG, Raine-Fenning N, Coomarasamy A. The prevalence of congenital uterine anomalies in unselected and high-risk populations: A systematic review. Hum Reprod Update 2011;17(6):761–71. [CrossRef]
[Pubmed]

10.
Homer HA, Li TC, Cooke ID. The septate uterus: A review of management and reproductive outcome. Fertil Steril 2000;73(1):1–14. [CrossRef]
[Pubmed]

11.
Nahum GG. Uterine anomalies. How common are they, and what is their distribution among subtypes? J Reprod Med 1998;43(10):877–87.
[Pubmed]

12.
Heinonen PK. Distribution of female genital tract anomalies in two classifications. Eur J Obstet Gynecol Reprod Biol 2016;206:141–6. [CrossRef]
[Pubmed]

13.
Brody JM, Koelliker SL, Frishman GN. Unicornuate uterus: Imaging appearance, associated anomalies, and clinical applications. AJR Am J Roentgenol 1998;171(5):1341–7. [CrossRef]
[Pubmed]

14.
Chopra S, Keepanasseril A, Rohilla M, et al. Obstetric morbidity and the diagnostic dilemma in pregnancy in rudimentary horn: Retrospective analysis. Arch Gynecol Obstet 2009;280(6):907–10. [CrossRef]
[Pubmed]

15.
Cobec IM, Seropian P, Rempen A. Pregnancy in a non-communicating rudimentary horn of a unicornuate uterus. Hippokratia 2019;23(2):92–4.
[Pubmed]

16.
Khati NJ, Frazier AA, Brindle KA. The unicornuate uterus and its variants: Clinical presentation, imaging findings, and associated complications. J Ultrasound Med 2012;31(2):319–31. [CrossRef]
[Pubmed]

17.
O’Leary JL, O’Leary JA. Rudimentary horn pregnancy. Obstet Gynecol 1963;22:371–5.
[Pubmed]

18.
Heinonen PK. Clinical implications of the unicornuate uterus with rudimentary horn. Int J Gynaecol Obstet 1983;21(2):145–50. [CrossRef]
[Pubmed]

19.
20.
Khati NJ, Frazier AA, Brindle KA. The unicornuate uterus and its variants. Clinical presentation, imaging findings, and associated complications. J Ultrasound Med 2012;31(2):319–31.
[Pubmed]

21.
Reichman D, Laufer MR, Robinson BK. Pregnancy outcomes in unicornuate uteri: A review. Fertil Steril 2009;91(5):1886–94. [CrossRef]
[Pubmed]

22.
Heinonen PK. Unicornuate uterus and rudimentary horn. Fertil Steril 1997;68(5):224–30. [CrossRef]
[Pubmed]

23.
de Souza CS, Dorneles GG, Mendonça GN, et al. Pregnancy in non-communicating unicornuate uterus: Diagnosis difficulty and outcomes – A case report. Rev Bras Ginecol Obstet 2017;39(11):640–4. [CrossRef]
[Pubmed]

24.
Publications Committee, Society for Maternal-Fetal Medicine, Belfort MA. Placenta accreta. Am J Obstet Gynecol 2010;203(5):430–9. [CrossRef]
[Pubmed]

25.
Oral B, Guney M, Ozsoy M, Sonal S. Placenta accreta associated with a ruptured pregnant rudimentary uterine horn. Case report and review of the literature. Arch Gynecol Obstet 2001;265(2):100–2. [CrossRef]
[Pubmed]

26.
Pellerito JS, McCarthy SM, Doyle MB, Glickman MG, DeCherney AH. Diagnosis of uterine anomalies: Relative accuracy of MR imaging, endovaginal sonography, and hysterosalpingography. Radiology 1992;183(3):79–800. [CrossRef]
[Pubmed]

27.
Jayasinghe Y, Rane A, Stalewski H, Grover S. The presentation and early diagnosis of the rudimentary uterine horn. Obstet Gynecol 2005;105(6):1456–67. [CrossRef]
[Pubmed]

28.
Kriplani A, Relan S, Mittal S, Buckshee K. Pre-rupture diagnosis and management of rudimentary horn pregnancy in the first trimester. Eur J Obstet Gynecol Reprod Biol 1995;58(2):203–5. [CrossRef]
[Pubmed]

29.
Ghi T, Casadio P, Kuleva M, et al. Accuracy of three-dimensional ultrasound in diagnosis and classification of congenital uterine anomalies. Fertil Steril 2009;92(2):808–13. [CrossRef]
[Pubmed]

30.
Tsafrir A, Rojansky N, Sela HY, Gomori JM, Nadjari M. Rudimentary horn pregnancy: First-trimester prerupture sonographic diagnosis and confirmation by magnetic resonance imaging. J Ultrasound Med 2005;24(2):219–23. [CrossRef]
[Pubmed]

31.
Mavrelos D, Sawyer E, Helmy S, Holland TK, Ben-Nagi J, Jurkovic D. Ultrasound diagnosis of ectopic pregnancy in the non-communicating horn of a unicornuate uterus (cornual pregnancy). Ultrasound Obstet Gynecol 2007;30(5):765–70. [CrossRef]
[Pubmed]

32.
Graupera B, Pascual MA, Hereter L, et al. Accuracy of three-dimensional ultrasound compared with magnetic resonance imaging in diagnosis of Müllerian duct anomalies using ESHRE-ESGE consensus on the classification of congenital anomalies of the female genital tract. Ultrasound Obstet Gynecol 2015;46(5):616–22. [CrossRef]
[Pubmed]

33.
Bermejo C, Martínez Ten P, Cantarero R, et al. Three-dimensional ultrasound in the diagnosis of Müllerian duct anomalies and concordance with magnetic resonance imaging. Ultrasound Obstet Gynecol 2010;35(5):593–601. [CrossRef]
[Pubmed]

34.
Blancafort C, Graupera B, Pascual MÀ, Hereter L, Browne JL. Cusidó MT, Diagnosis and laparoscopic management of a rudimentary horn pregnancy: Role of three-dimensional ultrasound. J Clin Ultrasound 2017;45(2):112–5. [CrossRef]
[Pubmed]

35.
Mueller GC, Hussain HK, Smith YR, et al. Müllerian duct anomalies: Comparison of MRI diagnosis and clinical diagnosis. AJR Am J Roentgenol 2007;189(6):1294–302. [CrossRef]
[Pubmed]

36.
Behr SC, Courtier JL, Qayyum A. Imaging of Mullerian duct anomalies. RadioGraphics 2012;32(6):E233–50. [CrossRef]
[Pubmed]

37.
Ozeren S, Caliskan E, Corakci A, Ozkan S, Demirci A. Magnetic resonance imaging and angiography for the prerupture diagnosis of rudimentary uterine horn pregnancy. Acta Radiol 2004;45(8):878–81. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Acknowledgments
The authors wish to thank Dr. Ari Reiss for his kind assistance with assembling the team of authors for this project. We thank Elsevier for permission to reproduce the material included in Table 1 of this manuscript.
Author ContributionsBoris Sokolovski - Conception of the work, Design of the work, Acquisition of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Sobhi Abadi - Acquisition of data, Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Chen Ben David - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Amnon Amit - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ido Solt - Acquisition of data, Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Marcia C Javitt - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Boris Sokolovski et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.