|
Case Report
Bilateral axillary lymph node metastases of a serous ovarian carcinoma: A case report
1 MD in Obstetric Gynecology, Chu Ibn Rochd, Casablanca, Morocco
2 MD in Pathological Anatomy, Chu Ibn Rochd, Casablanca, Morocco
3 Professor in Pathological Anatomy, Chu Ibn Rochd, Casablanca, Morocco
4 Professor in Obstetric Gynecology, Chu Ibn Rochd, Casablanca, Morocco
Address correspondence to:
Faizi Issam
MD in Obstetric Gynecology, Chu Ibn Rochd, Casablanca,
Morocco
Message to Corresponding Author
Article ID: 100092Z08FI2021
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Issam F, Amjad H, Asmaa E, Samira B, Mustapha B, Mohamed E, Mohamed E. Bilateral axillary lymph node metastases of a serous ovarian carcinoma: A case report. J Case Rep Images Obstet Gynecol 2021;7:100092Z08FI2021.ABSTRACT
Breast and axillary nodes involvement in ovarian cancer is extremely rare. We report a case of solitary axillary lymph nodes metastasis from ovarian carcinoma in a 66-year-old woman, simultaneously diagnosed with the serous ovarian carcinoma. The diagnostic, therapeutic, and prognostic aspects as well as a review of the literature of this uncommon site of metastasis are discussed.
Keywords: Axillary lymph nodes, Case report, Metastases, Ovarian cancer
Introduction
Metastasis of ovarian or peritoneal serous carcinoma to the breast and/or axillary lymph nodes is a rare event, and occurs mostly at an advanced stage of cancer. Nevertheless, its recognition and distinction from mammary carcinoma are of great clinical importance because the treatment and prognosis differ significantly [1].
We report the case of a patient with serous ovarian carcinoma with isolated bilateral axillary synchronous metastases.
Case Report
Our patient H.M. is a 66-year-old married woman, who was complaining, 9 months ago, with an abdominal distension. She was treated from blood hyperpressure under amlodipine 5 mg for 10 years, and had no personal or family history of cancer.
Clinical exam showed an abdominal distension with Flank Dullness, no palpable mass or exteriorized bleeding was found.
An abdomino-pelvic CT scan revealed a mass measuring 40/23 mm of left ovarian origin with moderate ascites. CA 125 was at 521 U/mL.
The diagnostic laparoscopy showed a left ovarian tumor measuring 40/30 mm with peritoneal carcinoma deemed inoperable.
A biopsy of both right and left ovaries, parietal peritoneum and a sample of ascites fluid were performed.
Histological exam revealed a focal ovarian localization of undifferentiated and invasive serous carcinomatous proliferation.
The extension disease staging (thoraco-abdomino-pelvic CT scan) did not show any secondary location apart from multiple bilateral axillary and supracalvicular lymph nodes.
Our patient did not complain of any kind of pain or swallowing in the axillary area, and the clinical exam showed bilateral multiple axillary lymph nodes.
In front of these findings, a mammography with a mammary ultrasound were indicated The mammography revealed bilateral axillary lymph nodes, some of which are necrotic without any suspect abnormality in both breasts, with vascular rails-like (Figure 1).
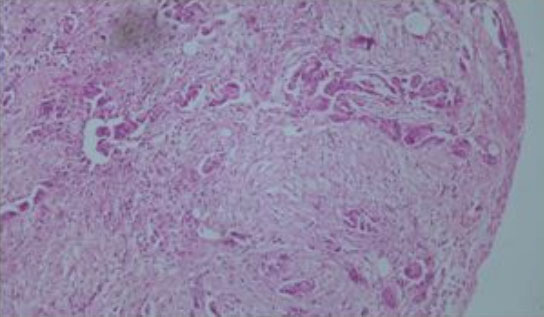
An axillary lymph node biopsy showed tumor proliferation arranged in spans and clumps and sometimes papillae. Tumor cells were pleomorphic with large hyperchromatic nuclei and a high nucleocytoplasmic ratio (Figure 2).
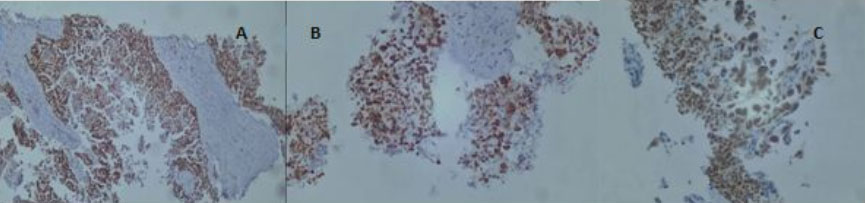
The immunohistochemical study showed tumor cells positive for WT1, P53, and PAX 8 and negative for GATA3, TTF1 (Figure 3).
In summary, it’s an axillary lymph nodes metastasis from ovarian carcinoma
The patient received eight cycles of paclitaxel and carboplatin. The follow-up CT showed a near-stable appearance of the ovarian mass as well as peritoneal carcinoma. CA 125 was at 126 U/mL vs 521 U/mL.
A second debulking surgery was proposed for the patient in which: a pelvic shield made the resectability impossible.
An evaluation CT scan was performed (nine months after the diagnosis) showed an increase in the volume of the tumor mass measuring 101×96 mm with persistence of peritoneal carcinoma and septate peritoneal effusion and upper right lobar pulmonary micronodule suspected as secondary nodes . The CA125 was at 1000. The patient was addressed for metastatic first-line chemotherapy made of gemcitabine, carboplatine and avastin.
Discussion
Although the primary mode of dissemination in ovarian carcinoma is intraperitoneal spread, ovarian cancer may also metastasize through lymphatic channels to the pelvic and para-aortic lymph nodes [2]. The rate of lymph node metastases of ovarian cancer differs according to histological type and stage of the tumor. Takeshima reported that the nodal involvement rate was lower in non-serous ovarian cancer [3]. Distant hematogenous metastases are in common in the presentation or during the disease. Dauplat et al. found that 38% of patients in their studies developed distant metastases [4].
As for our patient, no distant location was found except for the bilateral axillary lymph nodes. Metastases to the breast and axillary lymph nodes are rare. In large studies, they have been reported to constitute 0.4–2.0% of all breast malignancies [5]. The histological type most often found in this location is serous ovarian carcinoma reported in 72% of cases [6]. In addition, synchronous axillary lymph node involvement is seen in more than 60% of these patients. Few cases of isolated axillary lymph nodes metastases have been reported, as such as our case [1].
Metastatic axillary lymph nodes detected before or simultaneously with the ovarian tumor may have either an ovarian or mammary origin. The fear of missing out on a synchronous primary mammary carcinoma makes the determination of tumor markers and an immunohistochemical study to identify the site of origin of great importance in this situation, with 86% sensitivity and 89% specificity [7].
The pathologist should be informed of the existence of the primary tumor. Usually, histology can easily differentiate between lesions of metastatic origin and those of primary origin. Unlike primary breast tumors, breast metastases are generally well limited and appear to displace the mammary ducts rather than originate from them [8].
Tumor markers may also be helpful in establishing the primary site of tumor origin [9]. Gross cystic disease fluid protein-15 (GCDFP-15), a well-known marker of apocrine differentiation, has been reported as a highly specific and sensitive marker for breast cancer.
Expressions of GCDFP-15 and estrogen or progesterone receptors are important in distinguishing between the metastatic axillary lymph nodes as to whether they are derived from breast or ovary [10]. Another key chemical marker in the diagnosis of primary origin is WT-1.
The WT-1 gene is a tumor suppressor gene located on chromosome 11 at p1311. Al-Hussaini et al. found 94.7% of ovarian serous carcinomas [11], this is also the case with our patient.
When metastatic axillary lymph nodes are found in patients with ovarian carcinoma, treatment is of obvious importance. Breast metastases must be differentiated from primary breast carcinomas, as the prognosis and treatment are significantly different. If these lesions turn out to be metastatic, this will save the patient from unnecessary surgery and radiation therapy, and the clinician may be satisfied with chemotherapy as a palliative treatment [12].
Although it seems that recurrence of lymph nodes can lead to surgery with systemic treatment. Panici et al. [13] suggest systematic axillary lymphadenectomy in these patients and in the context of improving overall survival.
With an average overall survival of 26 months, patients who have presented with breast and/or axillary metastases have a poor prognosis, a result which was retaliatory in two other studies concerning this kind of metastasis [14], [15].
Conclusion
This case reports synchronous axillary metastasis of serous ovarian carcinoma which remains a rare entity, very difficult to diagnose and treat. Metastasis to the breast and axillary lymph nodes from ovarian and peritoneal serous carcinomas is an uncommon event. Accurate diagnosis of these metastases is crucial because the prognosis and therapeutic approaches differ significantly from primary tumors. Clinical history, comparative histology between primary ovarian carcinoma and axillary/breast localization in addition to immunohistochemical studies are essential for diagnosing metastases of ovarian origin, thus allowing an adequate therapeutic approach. The treatment is palliative. It is based on surgery and chemotherapy.
REFERENCES
1.
Recine MA, Deavers MT, Middleton LP, Silva EG, Malpica A. Serous carcinoma of the ovary and peritoneum with metastases to the breast and axillary lymph nodes: A potential pitfall. Am J Surg Pathol 2004;28(12):1646–51. [CrossRef]
[Pubmed]

2.
Aydin C, Unalp HR, Baloğlu A, Inci AG, Yiğit S, Yavuzcan A. Axillary lymph node metastasis from serous ovarian cancer: A case report and review of the literature. Arch Gynecol Obstet 2009;279(2):203–7. [CrossRef]
[Pubmed]

3.
Takeshima N, Hirai Y, Umayahara K, Fujiwara K, Takizawa K, Hasumi K. Lymph node metastasis in ovarian cancer: Difference between serous and non-serous primary tumors. Gynecol Oncol 2005;99(2):427–31. [CrossRef]
[Pubmed]

4.
Dauplat J, Hacker NF, Nieberg RK, Berek JS, Rose TP, Sagae S. Distant metastases in epithelial ovarian carcinoma. Cancer 1987;60(7):1561–6. [CrossRef]
[Pubmed]

5.
Raptis S, Kanbour AI, Dusenbery D, Shakir AK. Fine-needle aspiration cytology of metastatic ovarian carcinomas to the breast. Diagn Cytopathol 1996;15(1):1–6. [CrossRef]
[Pubmed]

6.
McIntoch IH, Hooper AA, Millis RR, Greening WP. Metastatic carcinoma within the breast. Clin Oncol 1976;2(4):393–401.
[Pubmed]

7.
Cormio G, di Vagno G, Melilli GA, Loverro G, Cramarossa D, Selvaggi L. Ovarian carcinoma metastatic to the breast. Gynecol Obstet Invest 2001;52(1):73–4. [CrossRef]
[Pubmed]

8.
Williams SA, Ehlers RA 2nd, Hunt KK, et al. Metastases to the breast from nonbreast solid neoplasms: Presentation and determinants of survival. Cancer 2007;110(4):731–7. [CrossRef]
[Pubmed]

9.
Kaufmann O, Deidesheimer T, Muehlenberg M, Deicke P, Dietel M. Immunohistochemical differentiation of metastatic breast carcinomas from metastatic adenocarcinomas of other common primary sites. Histopathology 1996;29(3):233–40. [CrossRef]
[Pubmed]

10.
Ozmen V, Asoglu O. Karanlik H, Cabioglu N, Kecer M, Bakkaloglu H. Primary ovarian cancer presenting with axillary lymph node metastases: A report of two cases. Acta Chir Belg 2007;107(1):75–7. [CrossRef]
[Pubmed]

11.
Al-Hussaini M, Stockman A, Foster H, McCluggage WG. WT-1 assists in distinguishing ovarian from uterine serous carcinoma and in distinguishing between serous and endometrioid ovarian carcinomas. Histopathology 2004;44(2):109–15. [CrossRef]
[Pubmed]

12.
Ozsaran AA, Dikmen Y, Terek MC, Ulukus M, Ozdemir N, Orgüc S, Erhan Y. Bilateral metastatic carcinoma of the breast from primary ovarian cancer. Arch Gynecol Obstet 2000;264(3):166–7. [CrossRef]
[Pubmed]

13.
Benedetti Panici P, Perniola G, Angioli R, et al. Bulky lymph node resection in patients with recurrent epithelial ovarian cancer: Impact of surgery. Int J Gynecol Cancer 2007;17(6):1245–51. [CrossRef]
[Pubmed]

14.
Dursun P, Yanik FB, Kuscu E, Gultekin M, Ayhan A. Bilateral breast metastasis of ovarian carcinoma. Eur J Gynaecol Oncol 2009;30(1):9–12.
[Pubmed]

15.
Karam AK, Stempel M, Barakat RR, Morrow M, Gemignani ML. Patients with a history of epithelial ovarian cancer presenting with a breast and/or axillary mass. Gynecol Oncol 2009;112(3):490–5. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Faizi Issam - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Harit Amjad - Acquisition of data, Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Elkebir Asmaa - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Benayad Samira - Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Benhessou Mustapha - Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ennachit Mohamed - Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Elkerroumi Mohamed - Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Faizi Issam et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.