|
Case Series
Cutaneous endometriosis: Symptomatic manifestation during pregnancy—A case series
1 MD, Resident Physician, Obstetrics and Gynecology, Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ, USA
2 MD, Assistant Professor, Obstetrics and Gynecology, Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ, USA
Address correspondence to:
Nadia Aurora
125 Paterson Street, New Brunswick, NJ 08901,
USA
Message to Corresponding Author
Article ID: 100100Z08NA2021
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Aurora N, Misra N. Cutaneous endometriosis: Symptomatic manifestation during pregnancy—A case series. J Case Rep Images Obstet Gynecol 2021;7:100100Z08NA2021.ABSTRACT
Introduction: Endometriosis is abnormal growth of uterine mucosal tissue outside of the uterus, and is most commonly restricted to the pelvis. Cutaneous manifestations have been well documented, particularly in cesarean scars. This is the first report of symptomatic cutaneous endometriosis during pregnancy.
Case Series: A 22-year-old female and a 29-year-old female both underwent repeat cesarean sections. They each had noted enlarging mobile masses in the area of their scars that became progressively more painful as they became closer to term. During repeat cesarean section these masses were excised, and pathology was consistent with decidualized endometrial tissue.
Conclusion: Cutaneous endometriosis should be included in the differential diagnosis of any patient who presents with pain and/or a palpable mass in the abdominoperineal region, especially in those who have had previous gynecological surgery. Surgery remains the mainstay of treatment. Complete excision prevents recurrence and should be the goal of treatment.
Keywords: Abdominal wall endometrioma, Cutaneous endometriosis, Incisional endometriosis, Pregnancy
Introduction
Endometriosis is abnormal growth of uterine mucosal tissue outside of the uterus and is most commonly restricted to the pelvis resulting in pelvic pain, dysmenorrhea, dyspareunia, and dyschezia [1]. Cutaneous endometriosis, though uncommon, has been documented for several decades [2],[3],[4]. Previously reported cases have described cutaneous manifestations as mobile masses within the skin layers with varying presentations of symptoms. Many lesions were noted within or in close proximity to scars from abdominal surgery, most commonly with Pfannenstiel incisions made for cesarean deliveries [5]. This report will discuss two separate patients who noted cyclical pain prior to their pregnancies. During pregnancy both then developed enlarging and painful cutaneous lesions in the area of their cesarean scars which were excised at the time of delivery and demonstrated histologic findings consistent with cutaneous endometriosis.
Case Series
Case 1
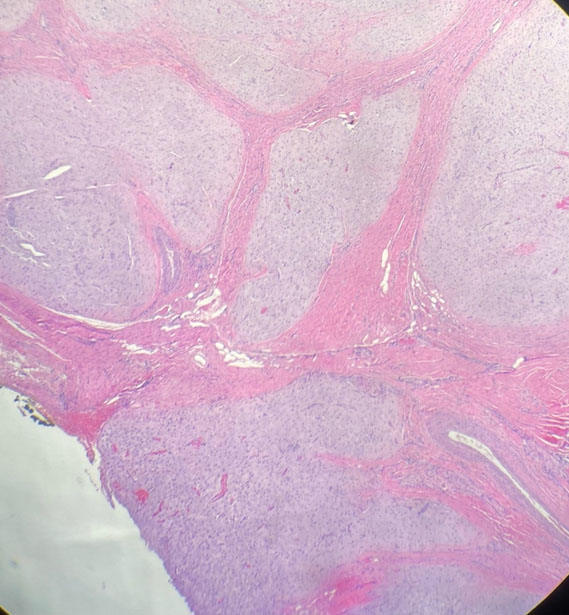
A 22-year-old female G2P1001 who had one previous cesarean delivery developed an enlarging and painful cutaneous lesion during pregnancy. At the time of delivery the lesion was 4 cm in diameter, mobile, with no other overlying skin changes. She presented at 38 weeks’ gestation with clinical signs concerning for labor as well as appendicitis. She underwent an uncomplicated repeat cesarean section with appendectomy and excision of a 4-cm subcutaneous mass to the right of midline in the area of her previous cesarean section scar. Her postoperative course was uncomplicated. The pathology (Figure 1 and Figure 2) demonstrated areas of well-circumscribed decidual tissue, at places extending into adipose tissue as well as skeletal muscle.
Case 2
A 29-year-old female G2P1001 had a mobile mass on the left aspect of her cesarean scar. She and her provider noted that it became larger and more painful during the pregnancy. At 39 weeks’ gestation presented for her scheduled repeat cesarean section with bilateral tubal ligation. At the time of excision, it was noted to be approximately 4 cm in size, subcutaneous, with no identifiable involvement of the fascia. It was excised and had a glandular appearance to the surgeons. The final pathology (Figure 3) identified decidualized endometrial tissue and fibromuscular tissue.
Discussion
Cutaneous endometriosis has been well characterized and published, with an estimated incidence of presence in cesarean scars ranging from 0.03% to 0.47% [6],[7]. However, its presence in pregnancy is poorly documented and likely underreported [7],[8],[9]. Our cases are unique as both patients noted enlargement as well as pain with their masses during pregnancy.
It is hypothesized that subcutaneous endometriosis, especially cases associated with an abdominal scar, is due to mechanical transplant of the endometrium into a new location [6],[10]. This tissue then responds to hormone fluctuations leading to further decidualization, enlargement, and resultant symptoms [7]. Due to its uncommon and varied nature, cutaneous endometriosis in pregnancy offers a wide differential diagnosis. Both benign and malignant causes must be carefully considered given the gravity of treatment to both mother and fetus. Benign manifestations include keloid, abscess, lipoma, and hernia. Malignant causes include melanoma, sarcoma, and Sister Mary Joseph nodule, a metastasis of an intrabdominal malignancy. Cesarean sections place women at highest risk of developing cutaneous endometriosis [5], which was the common factor between our two patients in addition to cyclic pain prior to pregnancy.
To date this is the first published report that identifies symptomatic worsening of cutaneous endometriosis diagnosed during pregnancy. Previous reports of cases diagnosed in pregnancy did not identify symptoms, or symptomatic manifestations were identified prior to pregnancy [7],[8].
Excision is the mainstay of treatment of this condition. Local wide excision to ensure complete removal of the disease is curative. Perioperative treatment with GnRH agonists has been advocated for relief of symptoms, especially, if the masses are enlarging and are painful, though a higher recurrence rate has been reported following the treatment [11]. Since the exact depth of the cutaneous endometriosis can only be determined at the time of surgery, and complete excision is the only way to ensure a cure, it is essential to counsel patients preoperatively regarding the possibility of recurrence. Spontaneous endometriosis is not preventable—scar endometriosis is likely to be preventable. Hence, routine irrigation of the abdominal wall wound before wound closure following any uterine surgery has been recommended, to prevent implantation of endometriotic cells. Possibly, patients with severe disease have several manifestations of the disease and cutaneous endometriosis could be one of the many extragenital manifestations. Thus far, this association has not been reported by any other authors.
Our patients had excision of their nodules with good cosmetic and symptomatic outcome. They received counseling on the pathologic findings and will continued to be followed to identify any continued symptoms outside of pregnancy.
Conclusion
In conclusion, cutaneous endometriosis is an increasingly diagnosed and reported condition with various sites of presentation, the most common being the abdominal wall. Due to a variable presentation, a high index of suspicion is needed to make the diagnosis. The condition should be included in the differential diagnosis of any patient who presents with pain and/or a palpable mass in the abdominoperineal region, especially in those who have had previous gynecological surgery. While symptoms are classically cyclical, the diagnosis of cutaneous endometriosis must not be disregarded if cyclicity is not demonstrable. Surgery remains the mainstay of treatment. Complete excision prevents recurrence and should be the goal of treatment, even if it results in large fascial defects requiring more extensive closure.
REFERENCES
1.
Giudice LC. Clinical practice. Endometriosis. N Engl J Med 2010;362(25):2389–98. [CrossRef]
[Pubmed]

2.
Wolf GC, Singh KB. Cesarean scar endometriosis: A review. Obstet Gynecol Surv 1989;44(2):89–95. [CrossRef]
[Pubmed]

3.
Lopez-Soto A, Sanchez-Zapta MI, Martinez-Cenda JP, Ortiz Reina S, Bernal Mañas CM, Remezal Solano M. Cutaneous endometriosis: Presentation of 33 cases and literature review. Eur J Obstet Gynecol Reprod Biol 2018;221:58–63. [CrossRef]
[Pubmed]

4.
Vellido-Cotelo R, Muñoz-González JL, Oliver-Pérez MR, et al. Endometriosis node in gynaecologic scars: A study of 17 patients and the diagnostic considerations in clinical experience in tertiary care center. BMC Womens Health 2015;15:13. [CrossRef]
[Pubmed]

5.
Nominato NS, Spyer LFVS, Lauar I, Morais J, Maia L, Geber S. Caesarean section greatly increases risk of scar endometriosis. Eur J Obstet Gynecol Reprod Biol 2010;152(1):83–5. [CrossRef]
[Pubmed]

6.
Bekta? H, Bilsel Y, Sari YS, et al. Abdominal wall endometrioma; a 10-year experience and brief review of the literature. J Surg Res 2010:164(1):e77–81. [CrossRef]
[Pubmed]

7.
D’Agostino C, Surico D, Monga G, Palicellic A. Pregnancy-related decidualization of subcutaneous endometriosis occurring in a post-caesarean section scar: Case study and review of the literature. Pathol Res Pract 2019;215(4):828–31. [CrossRef]
[Pubmed]

8.
Fair KP, Patterson JW, Murphy RJ, Rudd RJ. Cutaneous deciduosis. J Am Acad Dermatol 2000;43(1 Pt 1):102–7. [CrossRef]
[Pubmed]

9.
Steck WD, Helwig EB. Cutaneous endometriosis. Clin Obstet Gynecol 1966;9(2):373–83. [CrossRef]
[Pubmed]

10.
Maggiore ULR, Ferrero S, Mangili G, et al. A systematic review on endometriosis during pregnancy: Diagnosis, misdiagnosis, complications and outcomes. Hum Reprod Update 2016;22(1):70–103. [CrossRef]
[Pubmed]

11.
Rivlin ME, Das SK, Patel RB, Meeks GR. Leuprolide acetate in the management of cesarean scar endometriosis. Obstet Gynecol 1995;85(5 Pt 2):838–9. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Nadia Aurora - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Neeti Misra - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Nadia Aurora et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.