|
Case Report
The twisted uterus: A rare presentation of uterine torsion
1 Obstetrics and Gynaecology Trainee, Department of Obstetrics and Gynaecology, Guy’s and St Thomas’ NHS Foundation Trust, London SE1 7EH, UK
2 Medical Student, Department of Life Sciences & Medicine, King’s College London, London WC2R 2LS, UK
3 Consultant, Early Pregnancy and Gynaecology Unit, Department of Gynaecology, Guy’s and St Thomas’ NHS Foundation Trust, London SE1 7EH, UK
4 Obstetrics and Gynaecology Fellow, Early Pregnancy and Gynaecology Unit, Department of Gynaecology, Guy’s and St Thomas’ NHS Foundation Trust, London SE1 7EH, UK
5 Consultant, Department of Radiology, Guy’s and St Thomas’ NHS Foundation Trust, London SE1 7EH, UK
Address correspondence to:
Madeleine Trowsdale Stannard
Department of Obstetrics and Gynaecology, Guy’s and St Thomas’ NHS Foundation Trust, London SE1 7EH,
UK
Message to Corresponding Author
Article ID: 100106Z08MS2022
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Trowsdale Stannard M, Whittaker M, Abdul Aziz N, Cloke B, Diab Y, Gaughran J, Jacques A, Holland T, Amin T. The twisted uterus: A rare presentation of uterine torsion. J Case Rep Images Obstet Gynecol 2022;8:100106Z08MS2022.ABSTRACT
Introduction: Uterine torsion is a rare gynecological emergency, defined as torsion of the uterus greater than 45° around its axis. Case reports describe torsion either in the gravid uterus or in postmenopausal women, yet rarely in the non-gravid, premenopausal uterus. This report describes the case of uterine torsion secondary to a large pedunculated fibroid in a 34-year-old nulliparous woman.
Case Report: The patient presented with sudden onset of severe left sided abdominal pain which started during mild exertion. On examination she had a tender uterus which was enlarged secondary to a known large pedunculated fibroid. A planned myomectomy had been delayed due to the COVID-19 pandemic. Her pain worsened and therefore she was admitted with a working diagnosis of either torsion of the pedunculated fibroid or fibroid degeneration. A magnetic resonance imaging (MRI) scan was obtained which suggested torsion of the uterus itself and she was therefore taken for laparotomy for detorsion and myomectomy. The uterus, fallopian tubes, and ovaries were conserved and she recovered well postoperatively.
Conclusion: While uterine torsion in the non-gravid, premenopausal uterus remains extremely rare, it is an important diagnosis for clinicians to consider. This report discusses the diagnostic challenge when faced with a non-specific presentation. Magnetic resonance imaging can be helpful but ultimate diagnosis is surgical. Conservation of the uterus following torsion was possible in this case, giving the chance of fertility preservation. Finally, as demonstrated here, the impact of the COVID-19 pandemic on health services has caused delays to surgery which have had life and fertility-threatening consequences.
Keywords: Fertility preservation, Fibroids, Uterine conservation, Uterine torsion
Introduction
Uterine torsion is a rare gynecological emergency, defined as torsion of the uterus greater than 45° around its axis [1]. Torsion up to 720° has been reported, most commonly around the isthmus of the uterus [1],[2],[3]. Factors increasing the risk of uterine torsion include structural anomalies that distort pelvic anatomy, such as pregnancy, uterine fibroids [4], ovarian cysts [5], and adnexal tumors, and ligamentous laxity in the pelvis [5],[6]. Multiple case reports have described torsion either in the gravid uterus [2],[6] or in postmenopausal women [7],[8],[9], yet rarely in the non-gravid, premenopausal uterus. To the best of our knowledge, there remains only a single case of uterine torsion in a premenopausal non-gravid woman in the literature, described in 1935 [1]. This report describes the case of uterine torsion secondary to a large pedunculated fibroid in a 34-year-old nulliparous woman.
Case Report
A 34-year-old nulliparous woman attended the Emergency Department (ED) with sudden onset of severe left sided abdominal pain which started during mild exertion. The pain was associated with anorexia and nausea without vomiting or a change in bowel habit. She was on day 14 of her menstrual cycle.
Her body mass index (BMI) was raised at 40 kg/m2 with centripetal adiposity and she did not have any other co-morbidities. She was not currently trying to conceive, but wished to retain fertility. She had a known large pedunculated fibroid arising from the fundus, measuring 180 × 170 × 100 mm. This fibroid had last been visualized with MRI 11 months previously during outpatient investigation for mild abdominal pain and pressure symptoms under the gynecology team. An elective myomectomy had been scheduled six months prior to this acute presentation, but surgery had been significantly delayed due to the COVID-19 pandemic.
On review by the gynecology team, the uterus was mobile and enlarged to 24 weeks gestation. There was exquisite tenderness over the fundus. Speculum examination was normal and her inflammatory markers were unremarkable (white cell count 9.6×109/L [normal range 4.0–11.0×109/L], and C-reactive protein 7 mg/L [normal range 0–4 mg/L]). Her pregnancy test was negative. Given that she was clinically well, she was discharged home with a presumed diagnosis of fibroid degeneration and a follow up transvaginal ultrasound scan (TV-US) the next day. However, she represented to ED with worsening pain and vomiting, causing significant distress, agitation, and an inability to remain still. She was therefore admitted for further assessment and management.
Transvaginal and transabdominal ultrasound scans (TA-US) were performed on admission but the views were suboptimal due to body habitus. The findings demonstrated an anteverted uterus with a normal cavity and endometrium. A large subserosal fibroid was seen extending to the left upper quadrant. Neither ovary could be visualized on TV-US or TA-US but there was evidence of a small amount of free fluid within the anterior and posterior pelvic compartments. There was no evidence of hydronephrosis or renal calculi. An abdominal X-ray showed a non-obstructive bowel gas pattern. An MRI pelvis with contrast was requested to facilitate the diagnosis.
Upon admission the initial working diagnosis was torsion of the fibroid itself; however, fibroid degeneration remained a possibility, and there was consideration for an ovarian cyst accident, or Mittelschmerz pain as she was mid-cycle. Non-gynecological causes including pancreatitis and bowel obstruction were also considered.
Initial management consisted of pain relief with opiate analgesia and rehydration with intravenous fluids. On day 4 of her admission, she became tachypnoeic and tachycardic. Blood tests found an increase in her white cell count from 9.6×109/L on admission, to 22.2×109/L [normal range 4.0–11.0×109/L], and of C-reactive protein from 7 mg/L to 557 mg/L [normal range 0–4 mg/L]. Infection was therefore suspected. Chest X-ray and urinedip were both unremarkable, hence broad-spectrum intravenous antibiotics were commenced as the source was unclear. She was given ciprofloxacin, metronidazole, and vancomycin due to penicillin allergy. In light of tachycardia and tachypnea she was also investigated for pulmonary embolism with computed tomography (CT) pulmonary angiogram—due to her raised BMI and period of immobility increasing her risk of venous thromboembolism—both of which were unremarkable.
The inpatient MRI obtained on day 6 of admission demonstrated significant interval enlargement of the fibroid from 180 × 100 × 170 mm to 236 × 141 mm, and of both ovaries to 56 mm (R) and 47 mm (L). Absence of enhancement after use of contrast suggested acute fibroid and ovarian infarction, together with myometrial edema. The uterus and adnexa demonstrated a distorted, twisted configuration suggestive of uterine torsion (Figure 1). Free intra-pelvic fluid was noted and concomitant small bowel obstruction was suspected. The delay in obtaining the MRI was due to the need for a bariatric MRI scanner. A contrast CT was performed which confirmed the findings of small bowel obstruction with three transition points. The patient was taken for an emergency midline laparotomy with involvement from both the gynecological and general surgical teams. Operative findings included free fluid in the abdomen and a 25 cm pedunculated fundal fibroid that was attached to the uterus by a 4 cm pedicle.
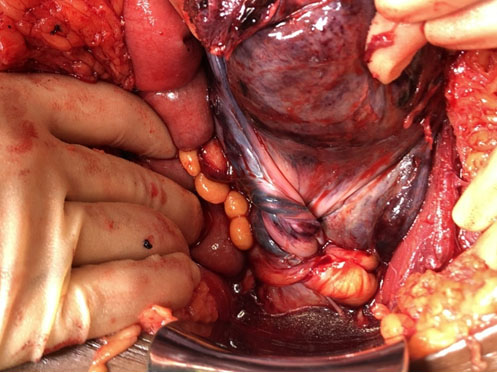
The fibroid was exteriorized and a myomectomy was performed. This revealed torsion of the uterus and adnexa by 720° clockwise on the isthmus of the uterus, with evidence of congestion and edema (Figure 2). The pelvic organs were detorted and conserved. The bowel was noted to be dilated but there were no signs of obstruction. Adhesiolysis was performed and a nasogastric tube inserted due to high risk of ileus.
Postoperatively the nasogastric tube remained in situ while electrolyte and fluid balance were closely controlled. On day 5 this was removed and a normal diet was gradually reintroduced. Analgesia was delivered via perioperative spinal anesthetic, rectus sheath catheters and patient-controlled analgesia until no longer required at five days postoperatively. Intravenous antibiotics were given for four days followed by an oral course for two weeks. Blood cultures showed no growth. We noted no immediate complications and she was discharged home 12 days following surgery.
Histopathology confirmed a leiomyoma with large areas of infarct-type necrosis, hyalinization and focal calcification. There was no evidence of malignancy. At the 6-week outpatient review, the patient was clinically well and pain free but menses had not resumed. She had no symptoms of premature ovarian insufficiency. A TV-US demonstrated a poor doppler uptake of the myometrium, and a heterogenous and thin endometrium. The right ovary was difficult to visualize, but the left was seen in the pouch of Douglas and had an antral follicle count of 8.
A hormonal profile was performed which showed: reduced anti-Müllerian hormone (AMH) level of <0.2 pmol/L [normal range 4.1–58.0 pmol/L], estradiol <92 pmol/L [normal range: follicular 98–571 pmol/L, ovulatory 177–1153 pmol/L, luteal 122–1094 pmol/L], follicle stimulating hormone (FSH) 60.0 IU/L [normal range: follicular 3.5–12.5 IU/L, luteal 1.7–7.7 IU/L], and luteinizing hormone (LH) 33.8 IU/L [normal range: follicular 2.4–12.6 IU/L, luteal 1.0–11.4 IU/L].
A postoperative MRI was performed four weeks later which showed hemorrhagic infarction and necrosis of the uterus and both ovaries, as a sequela of previous torsion. Repeat hormonal profile showed slight improvement: estradiol of 168 pmol/L, FSH of 38.6 IU/L, and LH of 26.5 IU/L. A repeat TV-US demonstrated a thin endometrium with normal vascularity in the cervix, but no vascularity above the cervix, nor in either ovary.
Discussion
Uterine torsion is a rare gynecological emergency. Risk factors include structural anomalies that distort pelvic anatomy, such as pregnancy, uterine fibroids [4], ovarian cysts [5] and adnexal tumors, and ligamentous laxity in the pelvis [6],[7]. Presentation is variable and often includes non-specific features, ranging from intermittent abdominal pain to acute deterioration with hemodynamic instability [8],[9],[10].
Association with nausea and vomiting, gastrointestinal and urinary symptoms, and vaginal bleeding have also been described [2]. Pregnant women may present with obstructed labor, fetal malpresentation, and fetal compromise [11], with diagnosis often made at caesarean section or exploratory abdominal surgery [12].
Diagnosis is challenging [13] and though imaging with the appropriate modality can be useful, it often requires review by an experienced clinician [3],[14]. The paucity in reports of uterine torsion in premenopausal non-gravid women is likely to be due to the rarity of this pathology, which in turn can lead to a limited awareness and delay in diagnosis. These factors contribute to poorer outcomes for women, with high rates of morbidity and mortality [12],[15]
The significant burden of disease associated with uterine torsion highlights the importance of clinicians’ ability to consider this diagnosis in women presenting with lower abdominal pain, especially in those who are pregnant or have a background of uterine pathology such as large fibroids or ovarian cysts. Accurate diagnosis and timely treatment are essential to achieving life and organ saving surgery.
Definitive management in the non-gravid uterus is usually with hysterectomy due to tissue infarction. In our case, the patients’ age, nulliparity, and desire to retain fertility weighed heavily in the decision-making process when deciding to conserve the uterus and ovaries. The congestion and edema of the pelvic anatomy noted at laparotomy brought into question whether she will be able to achieve a future pregnancy, but this was carefully balanced against the possibility that intervention with detorsion could increase her chance of successful conception. The immediate recovery period was uncomplicated, and it remains important to monitor her progress. However, the conclusions drawn from imaging and hormone levels at follow-up suggest that the uterine torsion will have long-term effects on her menstrual cycle and fertility, the implications of which have been explained to the patient.
Finally, an important reflection from this case was that of the impact of COVID-19 on health services, meaning that an elective myomectomy was postponed and the patient subsequently developed a life, organ, and fertility threatening condition. These severe consequences would most likely have been prevented with timely intervention and are an example of a wider secondary impact of the pandemic that requires public health attention.
Conclusion
This case report describes a 34-year-old woman with uterine torsion secondary to a large pedunculated fibroid. Uterine torsion in the non-gravid, premenopausal uterus remains extremely rare, but is an important diagnosis for clinicians to consider. As discussed, diagnosis can be challenging when faced with a non-specific presentation. This gynecological emergency can be suggested by magnetic resonance imaging but is ultimately diagnosed surgically. Conservation of the uterus following torsion was possible in this case, giving the chance of fertility preservation, although sadly her hormonal profile and imaging may suggest conception may not be possible, however time will tell. Finally, the impact of the COVID-19 pandemic on health services has caused delays to surgery which have had life and fertility-threatening consequences.
REFERENCES
1.
Hawes CH. Acute axial torsion of the uterus. Ann Surg 1935;102(1):37–40. [CrossRef]
[Pubmed]

2.
Jensen JG. Uterine torsion in pregnancy. Acta Obstet Gynecol Scand 1992;71(4):260–5. [CrossRef]
[Pubmed]

3.
Iraha Y, Okada M, Iraha R, et al. CT and MR imaging of gynecologic emergencies. Radiographics 2017;37(5):1569–86. [CrossRef]
[Pubmed]

4.
Sachan R, Patel ML, Sachan P, Arora A. Complete axial torsion of pregnant uterus with leiomyoma. BMJ Case Rep 2014;2014:bcr2014205558. [CrossRef]
[Pubmed]

5.
Chua KJ, Patel R, Eana A, Varughese J. Uterine torsion with necrosis of bilateral adnexa in a postmenopausal woman. BMJ Case Rep 2019;12(6):e229311. [CrossRef]
[Pubmed]

6.
Wang G, Ishikawa H, Sato A, Shozu M. Torsion of a large myomatous uterus associated with progressive renal failure and paralytic ileus in an 86-year-old woman. Case Rep Obstet Gynecol 2019;2019:1601368. [CrossRef]
[Pubmed]

7.
Oda H, Yamada Y, Uehara Y, et al. Uterine torsion in an elderly woman associated with leiomyoma and continuously elevating muscle enzymes: A case study and review of literature. Case Rep Obstet Gynecol 2020;2020:8857300. [CrossRef]
[Pubmed]

8.
Sikora-Szczęśniak D, Szczęśniak G, Łęgowik T, Sikora W. Torsion of the uterus with myomas in a postmenopausal woman - Case study and review of the literature. Prz Menopauzalny 2014;13(2):145–9. [CrossRef]
[Pubmed]

9.
Hashimoto A, Takahama J, Harada N, et al. A case of uterine torsion concurrent with a ruptured ovarian endometrial cyst. Abdom Radiol (NY) 2016;41(9):1707–12. [CrossRef]
[Pubmed]

10.
11.
Moores KL, Wood MG, Foon RP. A rare obstetric emergency: Acute uterine torsion in a 32-week pregnancy. BMJ Case Rep 2014;2014:bcr2013202974. [CrossRef]
[Pubmed]

12.
Wilson D, Mahalingham A, Ross S. Third trimester uterine torsion: Case report. J Obstet Gynaecol Can 2006;28(6):531–5. [CrossRef]
[Pubmed]

13.
Kremer JA, van Dongen PW. Torsion of the pregnant uterus with a change in placental localization on ultrasound; A case report. Eur J Obstet Gynecol Reprod Biol 1989;31(3):273–5. [CrossRef]
[Pubmed]

14.
Cheong EHT, Tan TJ, Wong KM. Torsion of a myomatous, non-gravid uterus: CT findings. J Radiol Case Rep 2018;12(4):6–14. [CrossRef]
[Pubmed]

15.
Lianga R, GandhI J, Rahmania B, Khan SA. Uterine torsion: A review with critical considerations for the obstetrician and gynecologist. Translational Research in Anatomy 2020;21(2):100084. [CrossRef]

SUPPORTING INFORMATION
Acknowledgments
The authors would like to thank the patient for giving consent to share her story.
Author ContributionsMadeleine Trowsdale Stannard - Conception of the work, Design of the work, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Maya Whittaker - Conception of the work, Design of the work, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Natasha Abdul Aziz - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Brianna Cloke - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Yasser Diab - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Jonathan Gaughran - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Audrey Jacques - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Tom Holland - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Tejal Amin - Conception of the work, Design of the work, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2022 Madeleine Trowsdale Stannard et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.