|
Case Report
A case of vulvar tumoral/vegetative herpes infection in an immunocompromised patient
1 Medical student, Albany Medical College, Albany, NY, USA
2 Associate Professor of Ob-Gyn, Department of Obstetrics and Gynecology, Oregon Health Sciences University, Portland, OR, USA
3 Professor of Dermatology and Pathology, Department of Dermatology and Pathology, University of Rochester School of Medicine, Rochester, NY,, USA
Address correspondence to:
Glynis Scott
MD, Box 601, Department of Dermatology, University of Rochester School of Medicine, Rochester, NY 14642,
USA
Message to Corresponding Author
Article ID: 100111Z08SS2022
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Scott S, Bonham A, Scott G. A case of vulvar tumoral/vegetative herpes infection in an immunocompromised patient. J Case Rep Images Obstet Gynecol 2022;8:100111Z08SS2022.ABSTRACT
Diagnosis of genital herpes is generally straightforward, allowing for prompt treatment. However, genital herpes may rarely present as large vegetative plaques, also known as “tumoral herpes” or “vegetative herpes,” mimicking malignancy, most commonly in patients infected with the HIV-AIDS virus. Tumoral/vegetative herpes (TVH) in renal transplant patients are rare. An 85-year-old woman with a history of renal transplant presented with a 1-year history of large painful vulvar masses. On exam, the patient had multiple exophytic lesions over the right labia majora extending to the perineum. A wide local excision was performed. Pathology revealed an exophytic lesion with abundant dermal inflammation. The epidermis showed scattered herpetic inclusions within keratinocytes that stained positively for herpes simplex virus types 1/2. A diagnosis of TVH was made. We present this patient to alert the clinician that genital herpes may present as an exophytic mass mimicking malignancy, particularly in immunocompromised patients. While the majority of cases of TVH have been reported in patients infected with HIV-AIDS, it is important to recognize that TVH may occur in other settings of immunocompromise, including patients with renal transplant.
Keywords: HSV, Immunosuppression, Transplant, Tumoral herpes, Vegetative herpes
Introduction
Herpes simplex viruses (HSV) are a large family of viruses that cause latent infection in their hosts. Diagnosis of HSV infection is typically straightforward in immunocompetent patients, who present with painful vesicles on mucocutaneous surfaces such as the mouth and genitals. In immunocompromised hosts, clinical presentation of infection with HSV is highly variable, and includes pustular or ulcerative lesions in unusual locations [1].
Genital herpes in immunocompromised patients rarely presents as large vegetative plaques, also known as tumoral or vegetative herpes (TVH), mimicking malignancy. This rare variant of genital herpes has been reported most frequently in patients infected with HIV-AIDS, but has also been reported in patients with lymphoma. Tumoral or vegetative herpes is thought to be a result of abnormal immune reaction to the herpes virus [2],[3],[4],[5]. To our knowledge, ours is the second report of a patient with genital TVH arising in a renal transplant patient [6].
Case Report
The patient is an 85-year-old woman with a complex past medical history including renal transplant in 2005, infiltrating ductal cancer of the left breast status post bilateral mastectomy in 2012, and diabetes. Medications include prednisone 5 mg every other day and acyclovir 1 g/day for a prior history of perianal herpes.
The patient presented to her gynecologist with a 1-year history of painful vulvar masses. A biopsy of the right labia majora was performed in January 2021 and was interpreted as “ulceration with granulation tissue and abscess.”
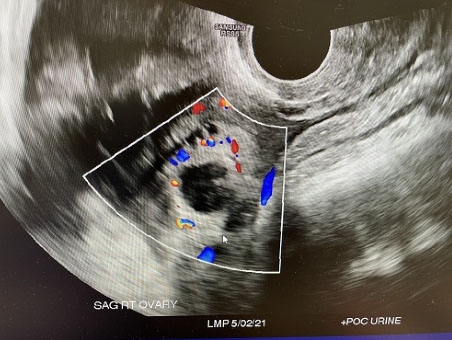
On exam the patient had multiple exophytic lesions over the right labia majora extending to the perineum (Figure 1). The largest lesion measured was 7×5 cm. There was a 4×3 cm lesion on the right perineum and a 7×2 cm lesion lateral to the right labia majora. Because of suspicion for occult malignancy not detected in the initial biopsy, a wide local excision was performed.
Review of the pathology revealed a large exophytic mass with abundant inflammation including lymphocytes and plasma cells in the dermis (Figure 2A). There was ulceration with herpetic inclusions noted within rare keratinocytes that stained positively for immunocytochemical stains against herpes simplex virus (Figure 2B and Figure 2C). Review of the initial biopsy revealed herpetic inclusions that had been missed by the original pathologist. A diagnosis of TVH was made.
Discussion
Tumoral/vegetative herpes is an uncommon manifestation of herpes simplex virus infection most frequently seen in patients with HIV-AIDS. In this report, we describe a patient with chronic immunosuppression secondary to renal transplant, with a prior history of perianal herpes infection, presenting with a vegetative mass that was misdiagnosed clinically as a malignancy. It should be noted that the patient was on acyclovir, consistent with known resistance of TVH to acyclovir, as well as other antivirals [7],[8].
Tumoral/vegetative herpes is a diagnostic pitfall for clinicians and pathologists. The initial biopsy of the lesion was misread as inflammatory, without note of the presence of typical herpetic viral inclusions within keratinocytes. Pathologists should be aware of TVH, as the predominant manifestation may be one of inflammation and fibrosis, with only scattered herpetic inclusions [3]. Tumoral/vegetative herpes is resistant to treatment with antivirals. Immune modulators, including imiquimod and surgical excision have been proposed as treatments [9],[10]. While TVH most commonly presents in patients with HIV-AIDS, clinicians should be aware that TVH can occur in other settings of immunocompromise, including chronic immunosuppressive therapy in renal transplant patients.
Conclusion
We present this patient to alert the clinician that genital herpes may present as an exophytic mass, particularly in immunocompromised patients. While the majority of cases of TVH have been reported in patients infected with HIV-AIDS, it is important to recognize that TVH may occur in other settings of immunocompromise, including patients with renal transplant.
REFERENCES
1.
Ljungman P. Herpes virus infections in immunocompromised patients: Problems and therapeutic interventions. Ann Med 1993;25(4):329–33. [CrossRef]
[Pubmed]

2.
Garib G, Hughey LC, Elmets, CA Cafardi JA, Andea AA. Atypical presentation of exophytic herpes simplex virus type 2 with concurrent cytomegalovirus infection: A significant pitfall in diagnosis. Am J Dermatopathol 2013;35(3):371–6. [CrossRef]
[Pubmed]

3.
Sasso BM, Florence MEB, Magalhaes RF, et al. Herpes simplex virus mucocutaneous tumoural lesions – Systematic review. J Clin Virol 2020;123:104246. [CrossRef]
[Pubmed]

4.
Ranu H, Lee J, Chio M, Sen P. Tumour-like presentations of anogenital herpes simplex in HIV-positive patients. Int J STD AIDS 2011;22(4):181–6. [CrossRef]
[Pubmed]

5.
Lautenschlager S, Schwarzkopf S, Keller B. Exophytic ulcerated tumors in HIV patients: Diagnostic and therapeutic problems. Dermatology 2008;216(1):60–3. [CrossRef]
[Pubmed]

6.
Hanjani NM, Foster DC, Scott GA, Mercurio MG. A genital mass due to herpes simplex virus in a renal transplant recipient. J Low Genit Tract Dis 2007;11(3):173–6. [CrossRef]
[Pubmed]

7.
Di Lucca-Christment J, Jacobelli S, Gressier L, et al. Anogenital pseudotumoral herpes and HIV infection: A new challenge for diagnosis and treatment. AIDS 2012;26(4):523–6. [CrossRef]
[Pubmed]

8.
Sbidian E, Battistella M, Legoff J, et al. Recalcitrant pseudotumoral anogenital herpes simplex virus type 2 in HIV-infected patients: Evidence for predominant B-lymphoplasmocytic infiltration and immunomodulators as effective therapeutic strategy. Clin Infect Dis 2013;57(11):1648–55. [CrossRef]
[Pubmed]

9.
Siqueira SM, Gonçalves BB, Loss JB, Estrella RR. Vegetative chronic genital herpes with satisfactory response to imiquimod. An Bras Dermatol 2019;94(2):221–3. [CrossRef]
[Pubmed]

10.
Chung VQ, Parker DC, Parker SRS. Surgical excision for vegetative herpes simplex virus infection. Dermatol Surg 2007;33(11):1374–9. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Samantha Scott - Conception of the work, Design of the work, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Adrienne Bonham - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Glynis Scott - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2022 Samantha Scott et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.