|
Case Report
Tubo-ovarian abscess in a virgin pediatric patient
1 School of Medicine, Loma Linda University, Loma Linda, CA, USA
2 Division of Pediatric Surgery, Loma Linda University Children′s Hospital, 11175 Campus Street, Room 21111, Loma Linda, CA, USA
3 Division of Obstetrics & Gynecology, Loma Linda University Medical Center, Loma Linda, CA, USA
Address correspondence to:
Andrei Radulescu
MD, PhD, FACS, Loma Linda University Medical Center, 11175 Campus Street, CP 21111, Loma Linda, CA 92350,
USA
Message to Corresponding Author
Article ID: 100067Z08LB2020
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Bathan L, Mendez YS, Sacks MA, Goodman L, Salcedo A, Hosseinifar N, Tagge E, Khan F, Radulescu A. Tubo-ovarian abscess in a virgin pediatric patient. J Case Rep Images Obstet Gynecol 2020;6:100067Z08LB2020.ABSTRACT
Introduction: Tubo-ovarian abscesses are rarely seen in non-sexually active patients, particularly because they lack the greatest risk factor: multiple sexual partners, avoiding genital tract infections, and subsequent tubo-ovarian abscesses.
Case Report: We present the case of a non-sexually active 15-year-old female, with a medical history of obesity, asthma, and diabetes, who presented to the Emergency Department (ED) with acute abdominal pain. Imaging studies (abdominal ultrasound (US) and computed tomography (CT)) suggested right ovarian torsion and she was taken urgently to the operating room for laparoscopic exploration. She did not have an ovarian torsion, but instead, a large right tubo-ovarian abscess and underwent surgical drainage.
Conclusion: This unique case presents a tubo-ovarian abscess in a virgin pediatric patient causing her abdominal pain.
Keywords: Abdominal pain, Pediatric, Tubo-ovarian abscess, Virgin
Introduction
Tubo-ovarian abscesses are serious and potentially life-threatening infections. When dealing with a pelvic mass, a tubo-ovarian abscess is just one potential diagnosis. Other diagnoses to consider include, but are not limited to ovarian tumor, ovarian or fallopian tube cyst, and ectopic pregnancy. Some of the most common factors that put women at greater risk for developing tubo-ovarian abscesses are reproductive age, multiple sexual partners, and prior history of upper genital tract infection or pelvic inflammatory disease. Tubo-ovarian abscesses are frequently polymicrobial, as both aerobes and anaerobes have been isolated. The classical presentation of women with tubo-ovarian abscesses includes acute lower quadrant abdominal pain, fever, chills, and vaginal discharge [1]. Treatment of tubo-ovarian abscesses generally begins with medical management through the administration of broad spectrum antibiotics, but, if necessary, surgical intervention is performed. In this case report, we present a rare and unique instance of a non-sexually active pediatric patient with a tubo-ovarian abscess.
Case Report
This is the case of a 15-year-old female who presented to the ED with right lower quadrant abdominal pain that started four days prior without an apparent precipitating factor. Her abdominal pain was accompanied by fever, malaise, nausea, vomiting, and anorexia. She has had no previous history of any similar episodes. Her past medical history was significant for obesity (BMI = 37.24 kg/m2), asthma and insulin dependent diabetes mellitus. Her last menstrual period had occurred two weeks prior to the visit. When questioned privately, she denied ever having engaged in any type of sexual activity. Her initial laboratory test results were significant for leukocytosis (WBC = 19.2 × 103/μL) with a neutrophilic shift (Neutrophils = 86.4%). In addition, her urine appeared cloudy and tested positive for protein, glucose, blood, ketones, leukocyte esterase, and bacteria. Her urine pregnancy test was negative. She then underwent imaging studies in the form of an US (Figure 1) and a CT scan (Figure 2). These demonstrated a large, inflamed, echogenic, hypoechoic mass with peripheral vascular flow and internal cystic regions on her right ovary, measuring 9.2 × 8.4 × 9.7 cm. Based on the US, a right ovarian torsion could not be ruled out. With the patient’s history of fever, presence of leukocytosis, and mass seen on imaging, the patient was seen by Pediatric Surgery and Adolescent Gynecological Surgery teams. After extensive discussion with patient and mother of diagnostic possibilities, potential effects on fertility, and the planned surgical procedure, an informed consent was signed.
The patient was urgently taken to the operating room for a diagnostic laparoscopy. Antibiotic therapy in the form of Doxycycline, Cefoxitin, and Flagyl were given intravenously prior to the surgical procedure. Initially, three 5 mm ports were placed in the umbilicus, left lower, and left lumbar quadrants. During laparoscopic visualization, the omentum was densely adherent to the entire pelvic opening. Lysis of adhesions reveals a firm inflammatory mass covered by omentum was in the right lower quadrant; however, it could not be separated from the underlying structures and so the ovaries could not be assessed for torsion. At this time, an additional port was placed in the right lower quadrant, improving visualization. As the inflammatory mass was mobilized, 150 cc of purulent fluid was drained from the abscess area. After drainage, pelvic structures were visualized as follows: bilateral hydrosalpinges, normal-appearing left ovary, unable to visualized right ovary, and soft, friable posterior uterine wall involved in the abscess. An intraoperative bimanual gynecology exam revealed an intact hymenal ring and vaginal discharge. This aided to mobilize the uterus and confirm anatomy. There was no disruption of ovaries or fallopian tubes; therefore, fertility should be preserved. All surgeons agreed with the diagnosis of a right tubo-ovarian abscess.
The abdomen was copiously irrigated and purulent fluid was sent for microbiological evaluation. An intraperitoneal 15 French Blake drain was then placed in the right lower quadrant. Postoperatively, she was admitted to the intensive care unit (ICU) for management of her elevated blood glucose with an insulin drip. She was also continued on antibiotics for an initially planned course of seven days. Cultures of the abscess grew gram positive bacilli resembling Lactobacilli and b hemolytic Group B Streptococci.
On postoperative day (POD) 3, she experienced a return of the abdominal pain and her laboratory test results showed a significant elevation in her white blood cell count (WBC = 21 × 103/μL), prompting concern for the recurrence of intra-abdominal pathology. Another CT scan was completed, which revealed a persistent right lower quadrant abscess. On POD 4, Interventional Radiology performed an ultrasound guided drainage of the abscess. Following this, her hospital course improved and she was discharged on POD 8.
Discussion
Tubo-ovarian abscesses generally occur as complications of pelvic inflammatory disease in sexually active patients. In these cases, the initial infection is caused by sexually transmitted pathogens entering from the lower reproductive tract and settling into the fallopian tubes and the ovaries. Frequently, these sexually transmitted pathogens include Escherichia coli, Aerobic Streptococci, Bacteroides fragilis, Prevotella, and Peptostreptococcus, but in rare instances, Candida species, Salmonella species, and Streptococcus pneumoniae have also been isolated [1].
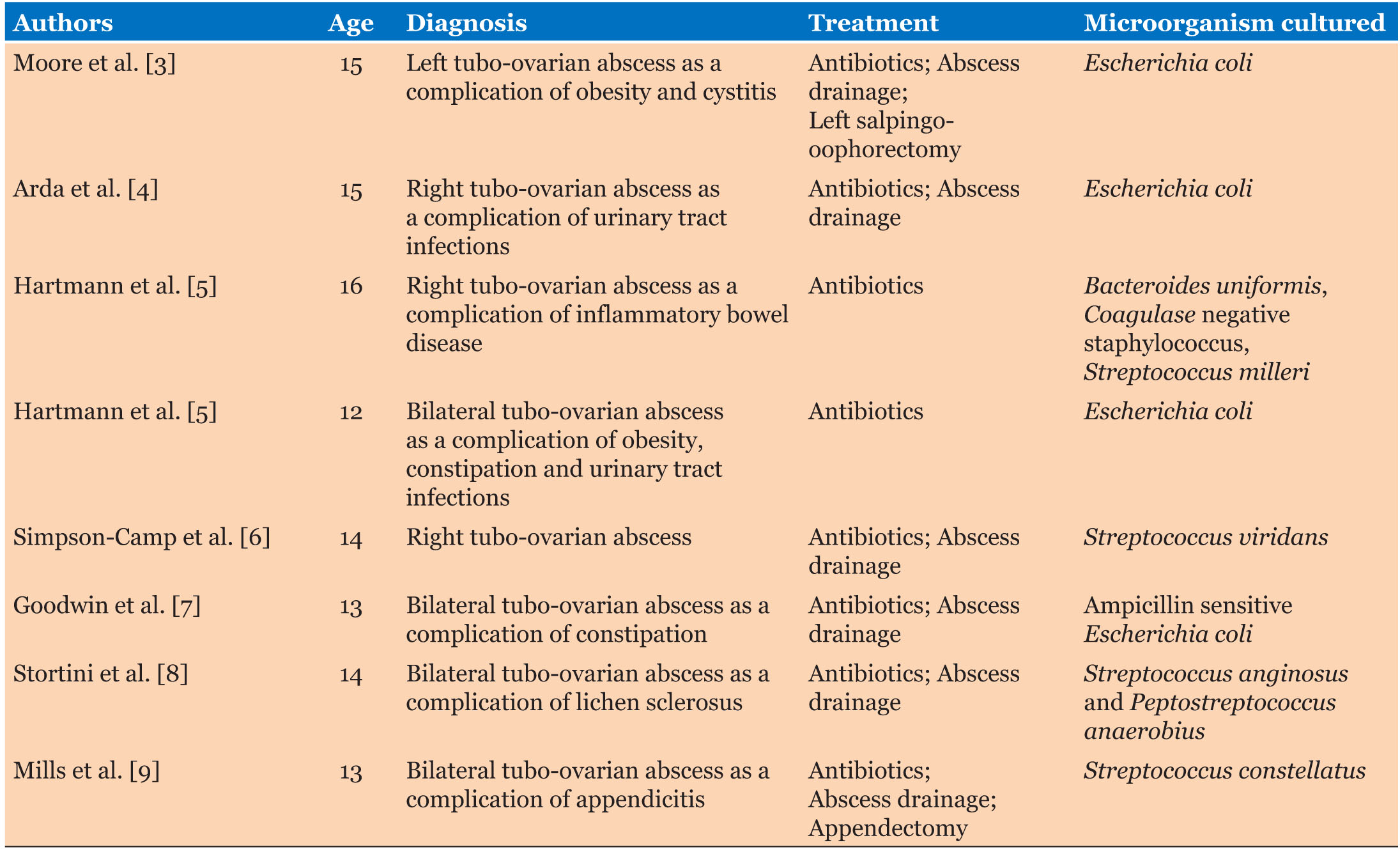
Although the majority of tubo-ovarian abscesses occur in sexually active patients, there are also documented cases of tubo-ovarian abscesses occurring in virgins and sexually inactive patients (Table 1), emphasizing the idea that sexual intercourse should not be considered a prerequisite in the development of tubo-ovarian abscesses [2],[3],[4],[5],[6],[7],[8],[9].
Following any diagnosis of tubo-ovarian abscess, there could be an impact on fertility. In discussing the impact on fertility, factors to consider include history of tubo-ovarian abscess, pelvic inflammatory disease, ectopic pregnancies, and surgeries required. Despite possible long-term effects on fertility, Rosen et al. showed an increase in achieving pregnancy from 4–15% to 32–63% with laparoscopic drainage over antibiotics alone [2]. Our patient will benefit in this way.
In these unique cases, the most prevalent presenting symptom was abdominal pain, but other common signs included tenderness, fever, and leukocytosis. Some of the hypothesized methods of infection, in these cases, included hematogenous spread of bacteria as a complication of inflammatory bowel disease [5], migration of bacteria from the urinary tract due to pooling of urine in the vagina as a result of a recessed urethra or agglutinated labia as well as urinary tract infections [3],[4],[5],[8], and translocation of bacteria from the gastrointestinal tract as a complication of constipation and appendicitis [7],[9]. Some of the atypical microorganisms isolated, in these cases, included Escherichia coli, Bacteroides uniformis, Coagulase negative staphylococcus, Streptococcus milleri, Streptococcus viridans, Streptococcus anginosus, Peptostreptococcus anaerobius, and Streptococcus constellatus [3],[4],[5],[6],[7],[8],[9].
In this case, cultures of the abscess grew gram-positive bacilli resembling Lactobacilli and b hemolytic Group B Streptococci, making this the first instance in which Lactobacilli and Group B Streptococci have been isolated from a tubo-ovarian abscess in a non-sexually active pediatric patient. Lactobacilli and Group B Streptococci are normal flora of the gastrointestinal tract and the female genital tract, but they can become pathogenic in certain circumstances. While infections caused by Lactobacilli and Group B Streptococci are extremely rare, the infections that they do cause generally occur in conjunction with an underlying medical condition, when the patient is in an immunocompromised state [10].
Based on this, we suspect that this patient developed the tubo-ovarian abscess through the spread of Lactobacilli and Group B Streptococci from either her gastrointestinal tract or her genitourinary tract, but the exact mechanism is uncertain. We also suspect that her diabetes played a role because diabetes is a risk factor of Lactobacilli and Group B Streptococci infections [11]. Because her diabetes was uncontrolled (HbA1C = 12.2%), we assumed that it may have promoted bacterial overgrowth within the gastrointestinal tract and/or genitourinary tract that ultimately translocated.
Overall, we believe that the diagnosis of tubo-ovarian abscess should be considered in patients presenting with abdominal pain, regardless of sexual history, because early treatment is crucial in preventing future complications, both acute and chronic, such as infertility, ectopic pregnancy, and pelvic pain [1],[3].
Conclusion
Tubo-ovarian abscesses can be seen in non-sexually active pediatric patients and, therefore, should be considered in the differential diagnoses, especially if the patient has additional risk factors.
REFERENCES
1.
Beigi RH, Epidemiology, clinical manifestations, and diagnosis of tubo-ovarian abscess. UpToDate 2020. [Available at: https://www.uptodate.com/contents/epidemiology-clinical-manifestations-and-diagnosis-of-tubo-ovarian-abscess]

2.
Rosen M, Breitkopf D, Waud K. Tubo-ovarian abscess management options for women who desire fertility. Obstet Gynecol Surv 2009;64(10):681–9. [CrossRef]
[Pubmed]

3.
Moore MM, Cardosi RJ, Barrionuevo MJ. Tubo-ovarian abscess in an adolescent virgin female. Arch Pediatr Adolesc Med 1999;153(1):91–2. [CrossRef]
[Pubmed]

4.
Arda IS, Ergeneli M, Coskun M, Hicsonmez A. Tubo-ovarian abscess in a sexually inactive adolescent patient. Eur J Pediatr Surg 2004;14(1):70–2. [CrossRef]
[Pubmed]

5.
Hartmann KA, Lerand SJ, Jay MS. Tubo-ovarian abscess in virginal adolescents: Exposure of the underlying etiology. J Pediatr Adolesc Gynecol 2009;22(3):e13–6. [CrossRef]
[Pubmed]

6.
Simpson-Camp L, Richardson EJ, Alaish SM. Streptococcus viridans tubo-ovarian abscess in an adolescent virgin. Pediatr Int 2012;54(5):706–9. [CrossRef]
[Pubmed]

7.
Goodwin K, Fleming N, Dumont T. Tubo-ovarian abscess in virginal adolescent females: A case report and review of the literature. J Pediatr Adolesc Gynecol 2013;26(4):e99–102. [CrossRef]
[Pubmed]

8.
Stortini B, Dural O, Kielly M, Fleming N. Tubo-ovarian abscess in a virginal adolescent with labial agglutination due to lichen sclerosus. J Pediatr Adolesc Gynecol 2017;30(6):646–8. [CrossRef]
[Pubmed]

9.
Mills D, Sharon B, Schneider K. Streptococcus constellatus tubo-ovarian abscess in a non-sexually active adolescent female. Pediatr Emerg Care 2018;34(6):e100–1. [CrossRef]
[Pubmed]

10.
11.
Sherid M, Samo S, Sulaiman S, Husein H, Sifuentes H, Sridhar S. Liver abscess and bacteremia caused by lactobacillus: Role of probiotics? Case report and review of the literature. BMC Gastroenterol 2016;16(1):138. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Lauren Bathan - Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Yomara S Mendez - Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Marla A Sacks - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Laura Goodman - Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Andrea Salcedo - Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Negar Hossinifar - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Edward Tagge - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Faraz Khan - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Andrei Radulescu - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2020 Lauren Bathan et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.