|
Case Report
Uterine artery pseudoaneurysm: A rare cause of delayed postpartum hemorrhage
1 Resident PGY2, Obstetrics and Gynecology, TriHealth Bethesda North Hospital, Cincinnati, Ohio, USA
2 Resident PGY3, Obstetrics and Gynecology, TriHealth Bethesda North Hospital, Cincinnati, Ohio, USA
3 Laborist Attending, Obstetrics and Gynecology, TriHealth Bethesda North Hospital, Cincinnati, Ohio, USA
Address correspondence to:
Morgan Wilhoite
DO, 13345 Princeton Lane, Pickerington, Ohio 43147,
USA
Message to Corresponding Author
Article ID: 100095Z08MW2021
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Wilhoite M, Parikh S, Holbert M. Uterine artery pseudoaneurysm: A rare cause of delayed postpartum hemorrhage. J Case Rep Images Obstet Gynecol 2021;7:100095Z08MW2021.ABSTRACT
Introduction: Uterine artery pseudoaneurysm (UAP) is a rare, life-threatening cause of secondary postpartum hemorrhage. The purpose of this case is to highlight the diagnosis and management of UAP, utility of imaging and uterine artery embolization, and the risk of infertility after fertility-sparing therapies.
Case Report: A 30-year-old G2P1011 presented with delayed postpartum hemorrhage after a cesarean section. Transvaginal ultrasonography (TVUS) illustrated a hypoechoic area with blood flow in a swirling pattern. Interventional radiology visualized a large right uterine artery pseudoaneurysm on angiography. A uterine artery embolization (UAE) was successfully performed with resolution of the patient’s symptoms.
Conclusion: Transvaginal ultrasonography is the diagnostic modality of choice when the cause of secondary postpartum hemorrhage is unclear. Uterine artery embolization can safely manage UAP without significant impact on conception or adverse obstetric outcomes.
Keywords: Embolization, Hemorrhage, Infertility, Pseudoaneurysm
Introduction
Postpartum hemorrhage (PPH) is a leading cause of maternal death worldwide. Delayed or secondary postpartum hemorrhage is defined as postpartum hemorrhage that occurs from 24 hours to 12 weeks postdelivery and affecting 0.23–3% of all deliveries, both vaginally and cesarean [1]. Causes of primary and secondary PPH differ in etiology and management. Most common causes of secondary PPH include abnormal involution of placental site, infection, and retained productions of conception.
Uterine artery pseudoaneurysm (UAP) is a rare and life-threatening cause that accounts for up to 3.3% of all known causes [2]. As the presentation of UAP can vary greatly, it is crucial to make an accurate diagnosis to avoid incorrect management and cause adverse outcomes. High clinical suspicion for UAP can lead to safe and efficient management while preserving a woman’s future fertility [2].
Case Report
We present a case of a 30-year-old G2P1011 African American patient admitted 10 days postpartum for heavy vaginal bleeding. Her pregnancy was complicated by anemia and obesity. She had an emergency cesarean section for a non-reassuring fetal heart rate tracing during her elective induction of labor. Her delivery was complicated by forceps assistance for delivery of fetal head and postpartum hemorrhage, with a quantitative blood loss of 2.26 L. She was not transfused with packed red blood cells during or after the procedure. Her postoperative hemoglobin and hematocrit (H&H) were noted to be 8.9 g/dL and 26.3%, respectively. Her postoperative course was otherwise uncomplicated and she was discharged home on iron supplements in stable condition on postoperative day 4.
The patient returned to triage on postpartum day 10 with an acute increase in vaginal bleeding. Her vitals were stable, she was afebrile, and asymptomatic aside from vaginal bleeding. Her physical exam was significant for her uterine fundus palpated above the level of the umbilicus but firm. Her pelvic exam was significant for bright red blood and clot filling the vaginal vault and speculum. A bedside transabdominal ultrasound (BSUS) was performed which showed an endometrial lining measuring 3.6 cm with heterogenous areas in the endometrial cavity, initially suspicious for retained products of conception. Her H&H on admission was unchanged from her prior admission and a plan was made for suction dilation and curettage in a controlled, non-emergent setting. With evidence of hemodynamic stability on presentation, decision was made to obtain a formal ultrasound in the morning and medically manage this patient with misoprostol and oxytocin overnight until her scan.
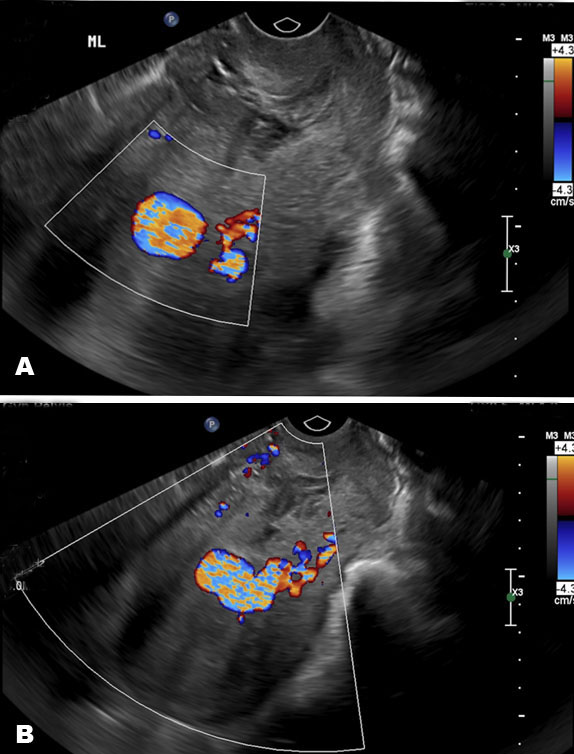
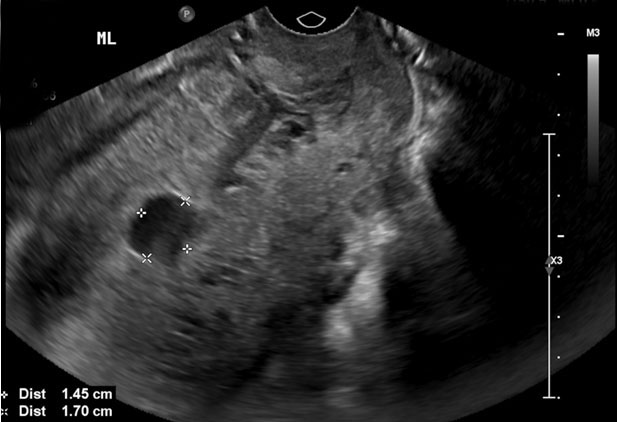
On hospital day 1, a repeat hemoglobin showed a slight drop from 8.9 g/dL on admission to 7.7 g/dL. She remained hemodynamically stable and only minimal vaginal bleeding was noted on physical exam. Findings from her formal pelvic ultrasound were concerning for a pseudoaneurysm as there was a hypoechoic area within the midportion of her uterus, extending into the endometrium and measuring 1.5×1.2×1.7 cm. Color flow Doppler showed a swirling of blood within this hypoechoic area and a connecting vessel in the left posterior aspect of the uterus (Figure 1 and Figure 2). Following interventional radiology consultation, decision was made to conservatively manage the uterine bleeding with uterine artery embolization to preserve fertility in this patient. Post-procedure findings were notable for a large pseudoaneurysm visualized from the right uterine artery. Gelfoam and 2 micro coils were utilized to achieve hemostasis in the right uterine artery.
The patient’s post-procedure course was complicated by acute blood loss anemia with a postoperative hemoglobin of 6.7 g/dL. She received two units of packed red blood cells with an appropriate rise in hemoglobin which remained stable. The patient was discharged on hospital day three in stable condition with plans for close follow-up.
Discussion
Uterine artery pseudoaneurysm is a rare etiology of secondary PPH that should be included in a differential diagnosis, as incorrect management can be deleterious. The common causes of delayed PPH, such as retained productions of conception, infection, or abnormal involution of the placental site, may prompt surgical management, which can lead to life and fertility threatening bleeding. In some cases, postpartum or postoperative bleeding complications may be a combination of subinvolution, retained products, UAP, etc. As in this case, Cytotec and Pitocin were administered on hospital readmission which could have played a role in controlling the patient’s bleeding if she were experiencing a combination of bleeding causes. This case report highlights the difficulty of clinical recognition of UAP as it often mimics more common causes of delayed PPH. Furthermore, this case brings attention to the use of transvaginal ultrasound with color Doppler as the imaging modality choice as well as using fertility sparing techniques to manage UAP in cases of delayed PPH [3],[4],[5],[6],[7].
Pathophysiology of pseudoaneurysm
An arterial pseudoaneurysm is a false aneurysm caused by trauma to the arterial wall. Compared to a true arterial aneurysm, pseudoaneurysms do not contain all three layers of the arterial wall (the adventitia, media, and intima). They are blood-filled cavities that vary in size and communicate with the lumen of their parent artery. When the arterial wall is injured, contact will be maintained with the parent vessel and extravasated blood will dissect through the arterial tissues [4]. For this reason, obstetricians and gynecologic surgeons will often identify pseudoaneurysms after instrumentation of the uterus during dilation and curettage, myomectomy, hysterectomy, operative (forceps) assisted deliveries, or cesarean sections. In the literature, it is estimated that post-cesarean delivery accounts for around 47.4% of all cases of UAP, making cesarean delivery the most common cause of UAP [5],[6]. As postoperative and postdelivery imaging is not routinely performed, it is difficult to estimate how many cases of asymptomatic UAP without vaginal bleeding go undetected.
Diagnosis of uterine artery pseudoaneurysm
Prior to management of postpartum hemorrhage, imaging should be performed to rule out UAP. As previously mentioned, the diagnostic imaging modality of choice is transvaginal ultrasonography with color Doppler [3],[4],[5],[6],[7]. On ultrasound Dopplers, a “to and fro” pattern may be visualized within a hypoechoic mass in the neck of the pseudoaneurysm [4]. The arterial blood will flow into the aneurysm cavity during systole and then reverse into the parent artery during diastole due to the pressure gradient. Other imaging modalities that can be diagnostic are magnetic resonance imaging and computed tomography with contrast.
Management of uterine artery pseudoaneurysm
There are various treatment approaches to the management of UAP; the patient’s preferences for future fertility should guide care in the shared-decision making process. For patients who are hemodynamically stable and desire fertility-sparing therapy, angiography is the gold standard as it is both diagnostic and therapeutic [8]. Interventional radiological uterine artery embolization (IR UAE) is a highly effective technique for controlling acute and chronic uterine bleeding. Benefits of this non-procedure include low complication rates, avoidance of surgical risks, shorter hospital stays, and fertility preservation.
A systematic review of the literature analyzing fertility following UAE illustrates that not only is conception possible, but also that pregnancy rates are comparable to the age-adjusted rates in the general population [9]. Some studies have reported high miscarriage rates following UAE along with other complications [10]. About 12.5% of pregnancies after UAE resulted in miscarriage and 87.5% resulted in successful live births between 36 to 39 weeks gestational age at delivery. The average time noted between embolization and conception was 23.8 months. Multiple studies note an increased risk of cesarean delivery in pregnancies following UAE [9],[10]. Furthermore, there were no statistically significant major obstetric risks to a pregnancy following UAE for delayed PPH, suggesting that pregnancy after UAE for PPH can occur without significant morbidity or mortality [3]. In studies of fertility and adverse pregnancy outcomes following UAE for uterine fibroids, it has been shown that there is a high rate for spontaneous abortion and malpresentation. However, these studies may not be applicable to cases as presented here, as fibroids can be independently associated with infertility and miscarriage [10].
Hemodynamically stable patients who desire fertility-sparing therapies should be offered IR UAE prior to invasive surgical management in nonmalignant pelvic bleeding [8]. Glue, polyvinyl alcohol particles, gelfoam, and micro coils are among the materials that can be used in IR embolization procedures with the most common of those materials used being polyvinyl alcohol particles [3]. The clinical success rate for gynecologic bleeding has been noted to be 91.9–96% with no recurrence of bleeding at a mean follow-up of 53 months after treatment [3]. Interventional radiological UAE has a recovery time of about 7–10 days and follow-up is needed to ensure bleeding resolution. For patients who need emergent treatment, as in those who are hemodynamically unstable, hysterectomy, removal of pseudoaneurysm, uterine vessel coagulation or ligation are viable options but may affect or eliminate a patient’s ability to conceive or carry a pregnancy in the future.
Conclusion
The case and literature presented above illustrate that all possible etiologies for delayed PPH should be considered prior to treatment. As this case highlights, failure to recognize rare vascular malformations, such as uterine artery pseudoaneurysms, may lead to life-threatening bleeding if incorrect management is undertaken. Thus, providers should have high clinical suspicion for rare causes of secondary PPH in patients with an abnormal presentation or workup. Ultrasound with color Doppler should be performed as the imaging modality of choice for the diagnosis of UAP. Depending on acuity and the patient’s desire for fertility preservation, a shared decision-making process is advisable. If fertility-sparing therapies are offered to patients, informed consent should include effects on future fertility. Based on the literature review provided in this case, patients should be counseled that while IR UAE may not result in decreased conception rates or adverse antepartum complications, it may be associated with an increase in the rate of cesarean delivery in any future pregnancies.
REFERENCES
1.
Patel N, Radeos M. Severe delayed postpartum hemorrhage after cesarean section. J Emerg Med 2018;55(3):408–10. [CrossRef]
[Pubmed]

2.
Dossou M, Debost-Legrand A, Déchelotte P, Lémery D, Vendittelli F. Severe secondary postpartum hemorrhage: A historical cohort. Obstetric Anesthesia Digest 2016;36(2):83–4. [CrossRef]

3.
Ghai S, Rajan DK, Asch MR, Muradali D, Simons ME, TerBrugge KG. Efficacy of embolization in traumatic uterine vascular malformations. J Vasc Interv Radiol 2003;14(11):1401–8. [CrossRef]
[Pubmed]

4.
Kurda D, Lukies M. Uterine artery pseudoaneurysm. Reference article, Radiopaedia.org. [Available at: https://radiopaedia.org/articles/38662]

5.
Kim YA, Han YH, Jun KC, Jeon MK, Lee ES. Uterine artery pseudoaneurysm manifesting delayed postabortal bleeding. Fertil Steril 2008;90(3):849. e11–4. [CrossRef]
[Pubmed]

6.
Isono W, Tsutsumi R, Wada-Hiraike O, Fujimoto A, Osuga Y, Yano T, Taketani Y. Uterine artery pseudoaneurysm after cesarean section: Case report and literature review. J Minim Invasive Gynecol 2010;17(6):687–91. [CrossRef]
[Pubmed]

7.
Sharma N Ganesh D, Devi L, Srinivasan J, Ranga U. Prompt diagnosis and treatment of uterine arcuate artery pseudoaneurysm: A case report and review of literature. J Clin Diagn Res 2013;7(10):2303–6. [CrossRef]
[Pubmed]

8.
Vedantham S, Goodwin SC, McLucas B, Mohr G. Uterine artery embolization: An underused method of controlling pelvic hemorrhage. Am J Obstet Gynecol 1997;176(4):938–48 [CrossRef]
[Pubmed]

9.
Bonduki CE, Feldner PC Jr, da Silva J, Castro RA, Sartori MGF, Girão MJBC. Pregnancy after uterine arterial embolization. Clinics (Sao Paulo) 2011;66(5):807–10. [CrossRef]
[Pubmed]

10.
Holub Z, Mara M, Kuzel D, Jabor A, Maskova J, Eim J. Pregnancy outcomes after uterine artery occlusion: Prospective multicentric study. Fertil Steril 2008;90(5):1886–91. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Acknowledgments
We would like to thank and acknowledge Dr. Samantha Mast, MD for reading the ultrasound report and reporting her suspicion for a pseudoaneurysm to the admitting team.
Author ContributionsMorgan Wilhoite - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Shivani Parikh - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Michael Holbert - Conception of the work, Design of the work, Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Morgan Wilhoite et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.