|
Case Report
Diagnosis of bilateral pseudoaneurysms of the uterine artery after laparoscopic uterine myomectomy
1 BA, Medical student, Ross University School of Medicine, Miramar, FL, USA
2 MD, Resident physician, Obstetrics & Gynecology, Mount Sinai South Nassau, Oceanside, NY, USA
3 MD, Attending physician, Obstetrics & Gynecology, Mount Sinai South Nassau, Oceanside, NY, USA; Associate professor, Obstetrics & Gynecology, Ross University School of Medicine, USA
Address correspondence to:
Beth Bentley
MD, 1 Healthy Way, Oceanside, NY 11572,
USA
Message to Corresponding Author
Article ID: 100098Z08DN2021
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Namburi D, Bentley B, Nguyen PC, Dean R. Diagnosis of bilateral pseudoaneurysms of the uterine artery after laparoscopic uterine myomectomy. J Case Rep Images Obstet Gynecol 2021;7:100098Z08DN2021.ABSTRACT
Introduction: Pseudoaneurysms of the uterine artery (UAP) are a rare cause of post-surgical vaginal hemorrhage. A pseudoaneurysm of the uterine artery is an extra-luminal collection of blood with turbulent flow that communicates with its parent vessel via a defect through the arterial wall.
Case Report: We present the case of a 36-year-old nullipara woman presenting 22 days post-laparoscopic uterine myomectomy. Her diagnosis of bilateral UAP was able to be determined via transvaginal Doppler ultrasound and confirmed via computed tomography (CT) angiography. Bilateral uterine artery embolization (UAE) was performed resulting in resolution of her symptoms.
Conclusion: Uterine artery pseudoaneurysm is a potentially life-threatening cause of post-surgical hemorrhage and should be considered as part of the diagnostic work up of post-operative vaginal bleeding. Uterine artery embolization is a safe and effective way to manage pseudoaneurysms of the uterine artery.
Keywords: Post-operative complication, Post-operative hemorrhage, Pseudoaneurysm, Uterine artery
Introduction
Pseudoaneurysm of the uterine artery can occur as a result of pelvic trauma, pelvic surgery, vaginal delivery, or cesarean section. Post-surgical and post-partum hemorrhagic complications can be classified in correspondence with their time of onset: early, occurring within the first 24 hours after surgery, or delayed, occurring after the first 24 hours of surgery and up to 6 weeks [1]. A postpartum delayed hemorrhage may be due to retained products of conception, endometritis, or inherited coagulopathies [1]. However, though uncommon, pseudoaneurysms of the uterine artery can present as delayed hemorrhage and should be considered as a cause of delayed hemorrhage in the post-surgical setting, due to the potential lethal consequences that can arise as a result [2].
Pseudoaneurysms of the uterine artery result from a defect in an arterial wall between the tunica media and tunica adventitia, which enable the formation of an extra-luminal hematoma with turbulent blood flow [3]. These defects are injuries that occur to the vessel wall from cesarean sections, vaginal deliveries, curettage, hysterotomy, or other pelvic surgeries [4]. Pseudoaneurysms of the uterine artery can present in a multitude of ways, ranging from asymptomatic and resolving independently to spontaneously rupturing allowing the possibility of life-threatening hemorrhage to occur, risk of which is dependent on the size of the defect and intraluminal pressure [4]. Ultimately, due to the serious effects that can arise, uterine artery pseudoaneurysms should be considered as a potential cause of delayed hemorrhage.
Case Report
This is a case of a 36-year-old nullipara female with a past medical history of thyroid disease who presented to our institution after an episode of acute vaginal bleeding with the passage of clots in conjunction with sharp lower abdominal pain. Records indicate that 22 days prior, at another institution, she underwent a laparoscopic uterine myomectomy and left ovarian cystectomy complicated by post-operative intra-abdominal bleeding requiring a subsequent exploratory laparotomy two days later. Operative reports state that 4000 mL were evacuated from the abdomen, and the source of bleeding was attributed to the posterior five centimeter sub-serosal myoma site, which was controlled by applying hemostatic agents and attaching the posterior cul de sac and serosa of the anterior rectum to the left adnexa. Post-operative computed tomography scan (CT) demonstrated a low attenuating lesion extending from the uterine fundus to the uterine body that was considered suspicious for laceration, and along the right uterine body a lobulated non-enhancing lesion (6.5 × 5.1 × 5.1 cm) consistent with a hematoma, in addition to a second complex cystic lesion in the right pelvis (3.3 × 2.6 × 3.3 cm) that was ascribed as being related to the adnexa or a possible second hematoma. A resultant CT angiogram was negative for any active bleeding and the patient was then discharged.
Nine days after her discharge, the patient re-presented to the Emergency Department (ED) due to fevers at home; however, repeat CT indicated an aging hematoma with a more linear lucency extending to the fundus likely related to her recent myomectomy, and the patient was discharged with ciprofloxacin and tylenol for a suspected urinary tract infection.
Seven days after her ED visit, she presented to our institution due to sudden onset uncontrollable vaginal bleeding with clots, in addition to a sharp lower abdominal pain that began eight hours prior. On physical exam the patient was febrile (37.9°C) and tachycardic (115 beats per minute). Inspection of the abdomen revealed a soft, non-distended abdomen, in conjunction with a well-healed non-erythematous midline incision. Bowel sounds were present and tenderness to deep palpation in the lower abdomen was demonstrated. Speculum exam displayed a closed cervix and 25 mL of dark red blood and clots. Bimanual exam showed uterine tenderness and cervical motion tenderness and a globular uterus approximately 14 weeks in size, with no adnexal masses palpated. Lab values demonstrated leukocytosis (WBC 20.2 K/ul), decreased hemoglobin (10.0 g/dL), thrombocytosis (PLT 465 K/ul), and an elevated absolute neutrophil count (17.3 K/ul).
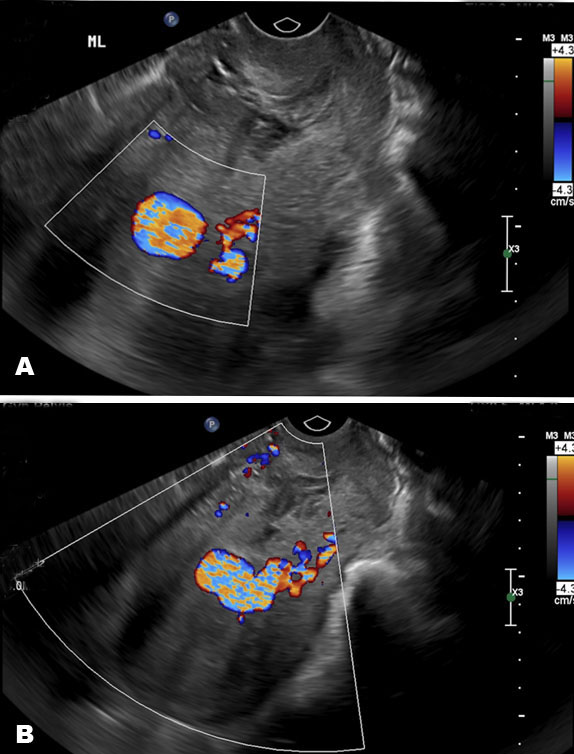
As a result of the patient’s presentation, a transvaginal and transabdominal pelvic ultrasound scan with color and spectral Doppler was ordered. Sonography reports indicated an anteverted uterus (10.6 × 6.5 × 8.5 cm) and a heterogenous solid and cystic myometrial mass (5.7 × 4.5 cm) within the anterior uterus. Right ovary was unremarkable, but the left ovary was unable to be identified, and a small amount of free fluid in the cul de sac (Figure 1). A CT was then ordered, revealing a complex fluid collection (6.7 × 7.2 × 4.7 cm) with an associated area of calcification (Figure 2).
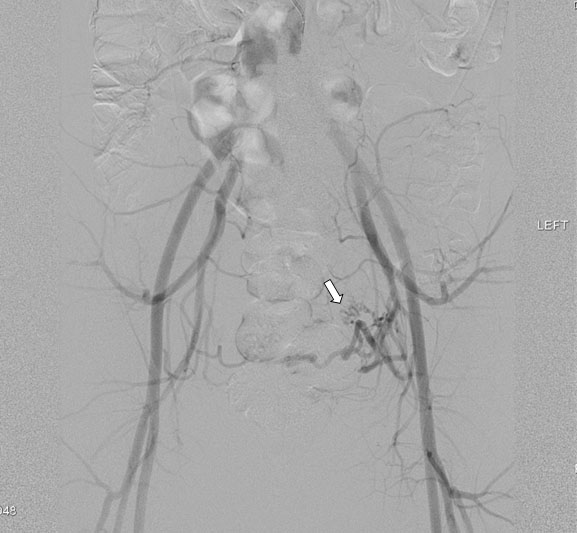
Upon review of the images with the interventional radiologist, the complex fluid collection was suspected to be a uterine artery pseudoaneurysm. Consequently, the patient was taken for a transcatheter UAE. Bilateral iliac angiography demonstrated tortuous bilateral uterine arteries with a rounded pseudoaneurysm being fed by both uterine arterial supplies (Figure 3). Subsequently, the left and right internal iliac arteries were both embolized via gelfoam temporary embolic, in order to preserve the patient’s fertility. Successful stasis was noted within both uterine arteries with no flow within the pseudoaneurysms, and flow was preserved bilaterally in the superior gluteal branches, external iliac, and femoral arteries.
The post-operative period was uneventful, and the patient was discharged the following day. She is being closely followed in regular periodic intervals by the gynecologic team.
Discussion
Pseudoaneurysm of the uterine artery is a rare cause of post-surgical hemorrhage; so rare that prevalence cannot be determined [5]. In this case, the patient presented to the hospital on two separate occasions before the diagnosis of uterine artery pseudoaneurysm was finally considered and diagnosed. Though any trauma to the arterial wall can result in a pseudoaneurysm, nearly half of all reported cases of UAP specifically arise post-cesarean section (47.4%) [6],[7]. Though uncommon, post-surgical pseudoaneurysms carry a 50% mortality rate, and therefore should be considered a potential diagnosis in delayed post-surgical hemorrhage [3].
Embolization of the uterine artery has become the dominant method of treatment of UAP, as the procedure carries a high success rate, and it enables the preservation of fertility [5]. However, though post-UAE of successful pregnancies has been demonstrated, studies have shown an increased rate of complications, including increased rates of cesarean section and miscarriage [8]. It has been hypothesized that these complications are due to decreased vascular supply to the endometrium causing complexities in maintaining the pregnancy or even potential difficulties in embryonic implantation [9],[10]. We hypothesize that bilateral pseudoaneurysms of the uterine arteries treated with UAE will increase complication rates in future pregnancies, compared to unilateral UAP. On review of the literature, there were no other cases of bilateral UAP described; therefore, we cannot determine absolute future consequences. Though UAE has become the leading treatment of pseudoaneurysms, they are contraindicated in hemodynamically unstable patients; unstable patients require emergent hysterectomy. Incidence of uterine artery ligation has been reported, but success rates are much poorer [1].
Conclusion
In conclusion, though pseudoaneurysms of the uterine artery are extremely rare, they are a potentially lethal complication of post-surgical vaginal bleeding and should therefore be considered as a potential diagnosis.
REFERENCES
1.
Samad S, Jonetzko P, Hawkins AP, Booth J, Thorpe-Beeston G, Marwood R. An unusual cause of delayed postpartum haemorrhage following caesarean section. Emerg Med J 2009;26(8):621–2. [CrossRef]
[Pubmed]

2.
Boi L, Savastano S, Beghetto M, Dall’Acqua J, Montenegro GM. Embolization of iatrogenic uterine pseudoaneurysm. Gynecol Minim Invasive Ther 2017;6(2):85–8. [CrossRef]
[Pubmed]

3.
4.
Subramaniam S, Nadarajan C, Aziz ME. Role of uterine artery embolization in pseudoaneurysm of uterine artery: A rare cause of secondary postpartum hemorrhage. Cureus 2018;10(2):e2220. [CrossRef]
[Pubmed]

5.
Parr K, Hadimohd A, Browning A, Moss J. Diagnosing and treating postpartum uterine artery pseudoaneurysm. Proc (Bayl Univ Med Cent) 2018;31(1):56–8. [CrossRef]
[Pubmed]

6.
Parvin A, Begum M, Huda A. Uterine artery pseudoaneurysm after cesarean section: Case report. Pulse 2015;7(1):56–60. [CrossRef]

7.
Schilke, Candice J, Michael KK. Pseudoaneurysm of the uterine arteries. Journal of Diagnostic Medical Sonography 2005;21:257–61. [CrossRef]
[Pubmed]

8.
Ugwumadu L, Hayes K, Belli AM, Heenan S, Loftus I. Uterine artery pseudoaneurysm requiring embolization in pregnancy: A case report and review of the literature. CVIR Endovasc 2018;1(1):31. [CrossRef]
[Pubmed]

9.
Ugwumadu L, Hayes K, Belli AM, Heenan S, Loftus I. Uterine artery pseudoaneurysm requiring embolization in pregnancy: A case report and review of the literature. CVIR Endovasc 2018;1(1):31. [CrossRef]
[Pubmed]

10.
Ciebiera M, Słabuszewska-Jóźwiak A, Zaręba K, Jakiel G. Management of uterine artery pseudoaneurysm: Advanced ultrasonography imaging and laparoscopic surgery as an alternative method to angio-computed tomography and transarterial embolization. Wideochir Inne Tech Maloinwazyjne 2017;12(1):106–9. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Deepa Namburi - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Beth Bentley - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Phuong Chi Nguyen - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Robert Dean - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Deepa Namburi et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.