|
Case Report
Heterotopic pregnancy managed laparoscopically and resulting in successful pregnancy outcome: A case report
1 Department of Obstetrics and Gynecology, Royal Devon University Healthcare Trust, Barnstaple, Devon, UK
Address correspondence to:
Yoseph Eskandar
Medical Student, Oxford University, Medical School, Oxford,
UK
Message to Corresponding Author
Article ID: 100156Z08YE2023
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Eskandar Y, Lekoudis E. Heterotopic pregnancy managed laparoscopically and resulting in successful pregnancy outcome: A case report. J Case Rep Images Obstet Gynecol 2023;9(2):12–15.ABSTRACT
Introduction: Spontaneous heterotopic pregnancy is extremely rare. It is diagnosed where at least two pregnancies are present simultaneously at different implantation sites, and where one of them is an intrauterine pregnancy. We present a case of heterotopic pregnancy which presented to the early pregnancy assessment clinic with abdominal discomfort at five weeks gestational age.
Case Report: A 32-year-old woman presented to the early pregnancy assessment clinic with lower abdominal pain. She was seen in the fertility clinic as she was trying to conceive for more than two years. She was para 2 having had 2 normal vaginal deliveries. She successfully achieved pregnancy on Clomid tablets 50 mg daily from day 2 to day 5 of the cycle. An ultrasound scan in the early pregnancy assessment clinic showed pregnancy of unknown location (PUL) with endometrial thickness of 10 mm at five weeks gestational age. She was subsequently diagnosed with heterotopic pregnancy with extrauterine mass measuring 1.64 cm in size. This was associated with an intrauterine sac with an embryo of about six weeks gestational age. She had laparoscopic right salpingectomy at gestational age of six weeks. She continued with her intrauterine pregnancy until term, and she had spontaneous normal vaginal delivery at 39+4 weeks.
Conclusion: Heterotopic pregnancy is a rare condition, estimated to occur in about 1/30,000 pregnancies. The most common extrauterine location of ectopic pregnancy is the fallopian tube although it can occur in other sites such as cervix, ovary, or anywhere intra-abdominally. Heterotopic pregnancy tends to be overlooked after confirming an intrauterine pregnancy; however, assessment of both adnexae is very important to exclude heterotopic pregnancy. Early detection and treatment of heterotopic pregnancy is key to prevent rupture of the ectopic pregnancy. This has significant consequences in maternal morbidity and mortality and, furthermore, increases the chance of intrauterine pregnancy continuing to term.
Keywords: Heterotopic pregnancy, Intrauterine pregnancy, Successful outcome
Introduction
Heterotopic pregnancy is a rare condition characterized by cooccurrence of two pregnancies in two different implantation sites, most commonly intrauterine and tubal pregnancy. It is estimated to occur in 1 in 30,000 spontaneous pregnancies. However, with assisted reproductive techniques an incidence of 1 in 100 pregnancies has been quoted in some literatures.
The diagnosis of the heterotopic pregnancy is based on the clinical picture, ultrasound scan, biochemical evaluation including serum β-hCG and magnetic resonance imaging (MRI). However, it can pose a significant challenge to diagnose such condition due to the complexity of clinical presentation, imaging interpretation, and laboratory findings [1].
Case Report
A 32-year-old woman was seen in the fertility clinic. She was para 2 having had 2 normal vaginal deliveries. She was trying to get pregnant for more than two years. Her hormonal profile luteinizing hormone/follicle stimulating hormone (LH/FSH) ratio was elevated suggesting polycystic ovarian syndrome (PCOS). She had a hysterosalpingogram (HSG) which was inconclusive suggesting some resistance on injecting the methylene blue dye; however, there was spillage and a picture suggestive of peri-tubal adhesions on the right side. Progesterone level at day 21 showed the low level of 10.9 nmol/L suggesting non-ovulation.
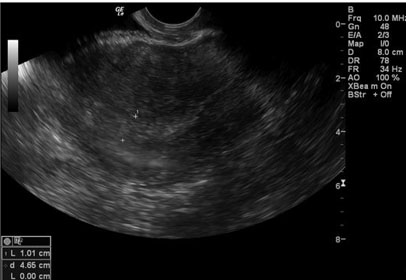
She was started on Clomid tablets 50 mg daily. Subsequent progesterone level was 62 nmol/L indicating ovulation. She successfully attained pregnancy after one cycle of this regime. She was seen in the early pregnancy assessment clinic (EPAC) with lower abdominal discomfort at five weeks gestational age. She had an ultrasound scan in the EPAC at five weeks which showed endometrial thickness of 10 mm; therefore, pregnancy of unknown location (PUL) was diagnosed (Figure 1).
She had another ultrasound scan a week later at six weeks gestational age which showed an intrauterine gestational sac of approximately 1.4 × 0.9 cm with yolk sac (Figure 2). The ultrasound scan also showed an extrauterine mass measuring 1.64 cm with a yolk sac and adjacent corpus luteum cyst (Figure 3). The ultrasound scan picture was suggestive of heterotopic pregnancy. The serum β-hCG was 2,586 at five weeks gestational age then 4,984 and then 11,302 U/L two days apart. Progesterone level was 106.7 nmol/L. She underwent diagnostic laparoscopy which confirmed right-sided fallopian tube ectopic pregnancy (Figure 4). She had laparoscopic right salpingectomy without manipulating the uterus vaginally. She recovered well and an ultrasound scan confirmed viable intrauterine pregnancy and was discharged home the next day postoperatively. The histopathology confirmed right ectopic pregnancy 45 × 20 mm in diameter (Figure 5).
The remainder of the pregnancy continued uneventfully (Figure 6) and she had a spontaneous normal delivery of a live baby boy at 39+4 weeks.
Discussion
Heterotopic pregnancy is defined as coexistence of at least 2 pregnancies in at least 2 different implantation sites. The most common sites of the heterotopic pregnancy are intrauterine pregnancy associated with tubal pregnancy [2]. However, other sites of ectopic pregnancy can occur such as ectopic cervical pregnancy, intra-abdominal pregnancy, cornual pregnancy, and ovarian pregnancy. Heterotopic pregnancy, also called heterotrophic pregnancy is extremely rare with a quoted incidence of 1/30,000 [3]. However, this incidence is underestimated particularly after introduction of assisted reproductive technologies (ART) [4].
The risk factors for heterotopic pregnancy are ART particularly in vitro fertilization (IVF), previous ectopic pregnancy, previous tubal or pelvic surgery, use of an intrauterine device and a history of pelvic inflammatory disease [5]. The diagnosis of ectopic pregnancy can be challenging due to variation in presentation; however, the aim of the early pregnancy assessment clinic is to diagnose ectopic pregnancy early to prevent the harmful health consequences of rupture of the ectopic pregnancy. Nevertheless, the diagnosis of heterotopic pregnancy is even more challenging. The presence of intrauterine pregnancy can give false reassurance and heterotopic pregnancy can be overlooked. Furthermore, the unpredicted levels of the serum β-human chorionic gonadotropin (β-hCG) due to the presence of two pregnancies in two different sites pose another challenge. The common association of corpus luteum cyst with normal pregnancy can be also misdiagnosed as heterotopic pregnancy and vice versa. In our case, a corpus luteum cyst was present adjacent to the ectopic tubal pregnancy (Figure 3). Another differential diagnosis that should be considered is ectopic pregnancy with an intrauterine pseudo-gestational sac [6]. All these represent challenges in diagnosing heterotopic pregnancy; however, early diagnosis is key for a successful continuation of the intrauterine pregnancy. Diagnosis of heterotopic pregnancy relies on ultrasound evaluation of an early gestation, clinical presentation, biochemical evaluation including serum β-hCG levels with a high index of clinical suspicion and awareness of the condition. However, MRI may be helpful in selected cases to confirm heterotopic diagnosis.
Management options of ectopic pregnancy in general are expectant, medical, and surgical options. In heterotopic pregnancy the management is mainly based on the surgical option. Expectant management is not ideal because of the challenges of the follow-up in terms of the level of the serum β-hCG with the ongoing intrauterine pregnancy. Medical management including systemic methotrexate is contraindicated because of its potential harmful effect on the viable intrauterine pregnancy [7]. The surgical management includes laparoscopy or laparotomy. The gold standard of the surgical management is laparoscopy depending on the clinical condition of the patient and the experience of the clinician. Laparoscopic salpingectomy is the recommended modality of treatment; however, salpingotomy can be considered in a few cases if the contralateral fallopian tube had been already damaged or removed. Nevertheless, follow-up for residual trophoblastic disease with serum β-hCG after salpingotomy is difficult with the ongoing intrauterine pregnancy. Furthermore, intraperitoneal irritation with salpingotomy may increase the risk to the intrauterine pregnancy which is another limitation when considering salpingotomy in treating heterotopic pregnancy [8].
Conclusion
Heterotopic pregnancy is a rare condition; however, it can be life-threatening due to delayed diagnosis because of the complexity of the clinical findings and interpretation of the investigations. High index of suspicion is required to achieve early diagnosis before rupture of the ectopic pregnancy with its sequelae of maternal morbidity and mortality. Furthermore, early diagnosis is essential to improve the outcome of the coexisting ongoing intrauterine pregnancy. Treatment of heterotopic pregnancy should be individualized; however, a laparoscopic approach is the mainstay in hemodynamically stable patients and salpingectomy is the preferred modality with a less invasive effect on the ongoing intrauterine pregnancy.
REFERENCES
1.
Ali T, Tawab MA, ElHariri MAG, Ayad AA. Heterotopic pregnancy: A case report. Egypt J Radiol Nucl Med 2020;51:214. [CrossRef]

2.
Soares C, Maçães A, Novais Veiga M, Osório M. Early diagnosis of spontaneous heterotopic pregnancy successfully treated with laparoscopic surgery. BMJ Case Rep 2020;13(11):e239423. [CrossRef]
[Pubmed]

3.
Reece EA, Petrie RH, Sirmans MF, Finster M, Todd WD. Combined intrauterine and extrauterine gestations: A review. Am J Obstet Gynecol 1983;146(3):323–30. [CrossRef]
[Pubmed]

4.
Clayton HB, Schieve LA, Peterson HB, Jamieson DJ, Reynolds MA, Wright VC. A comparison of heterotopic and intrauterine-only pregnancy outcomes after assisted reproductive technologies in the United States from 1999 to 2002. Fertil Steril 2007;87(2):303–9. [CrossRef]
[Pubmed]

5.
Ankum WM, Mol BW, Van der Veen F, Bossuyt PM. Risk factors for ectopic pregnancy: A meta-analysis. Fertil Steril 1996;65(6):1093–9.
[Pubmed]

6.
Weerakkody Y, Knipe H, Shah V, et al. Heterotopic pregnancy. Reference article, Radiopaedia.org. 31 Mar 2011. [Available at: https://radiopaedia.org/articles/13338] [CrossRef]

7.
Hutchinson M, Chan C. Laparoscopic management of ruptured heterotopic pregnancy after intrauterine insemination. CMAJ 2016;188(17–18):E525–7. [CrossRef]
[Pubmed]

8.
Abdelmonem AH, Sayed G, Abugazia AE, Kohla S, Youssef R. Heterotopic pregnancy after a spontaneous conception a case report with a review of clinical, laboratory and imaging findings. Clin Case Rep 2021;9(8):e04649. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Yoseph Eskandar - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Eleni Lekoudis - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2023 Yoseph Eskandar et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.