|
Case Report
Crepitus: A rare benign case of subcutaneous emphysema after abdominal myomectomy
1 Department of Obstetrics and Gynecology, Wayne State University/Detroit Medical Center, Detroit, Michigan, USA
Address correspondence to:
Richard Hsu
MD, Wayne State University/Detroit Medical Center, 3990 John R, 7-Brush N, Room 7613, Detroit, Michigan,
USA
Message to Corresponding Author
Article ID: 100157Z08RH2023
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Hsu R, Contos G. Crepitus: A rare benign case of subcutaneous emphysema after abdominal myomectomy. J Case Rep Images Obstet Gynecol 2023;9(2):16–18.ABSTRACT
Introduction: Postoperative crepitus is a rare finding following laparotomy cases. The potential diagnoses for this condition can vary from benign to high morbidity and mortality findings.
Case Report: In this case report, we discuss a case of a patient who developed non-specific abdominal pain who ultimately found to have crepitus on physical examination postoperative day 1. Subsequent computed tomography (CT) scan revealed a rare postoperative subcutaneous emphysema. Although these findings are infrequent after laparotomy, it is important to note that abdominal and incisional pain are commonly experienced symptoms after surgery.
Conclusion: This report aims to enhance postoperative care for patients who have undergone laparotomy.
Keywords: Crepitus, Gynecology surgery, Laparotomy, Subcutaneous emphysema
Introduction
Crepitus is a rare postoperative finding. Crepitus is a physical examination finding that represents an audible crackling and popping sensation with movement or palpation of body tissue. Differential diagnosis includes infection, such as necrotizing fasciitis, or operative complications, such as perforated viscus. Crepitus could represent benign findings for subcutaneous emphysema. In the literature to this date, there are less than five reported cases of benign subcutaneous emphysema. In most circumstances, subcutaneous emphysema is seen with laparoscopy given the use of carbon dioxide for insufflation. Here we describe a case of a patient who developed subcutaneous emphysema postoperatively from an abdominal myomectomy. This particular case highlights the importance of a comprehensive physical examination, immediate recognition of crepitus, and close monitoring of vitals and serial abdominal examinations.
Case Report
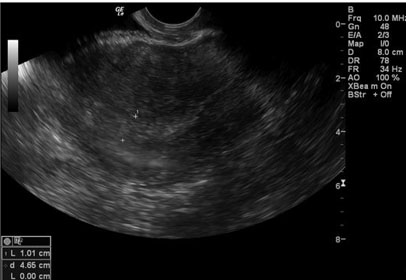
A 36-year-old, gravida 0, presented for schedule abdominal myomectomy for pelvic pain and abnormal uterine bleeding. The patient had no past medical history and no prior abdominal/thoracic surgical history. Transvaginal ultrasound demonstrated an enlarged globular heterogenous uterus with multilobulated contour measuring 13×5.5×5 cm. Hypoechoic solid myometrial masses were present—including an 8.8 cm fundal subserosal, 1.9 cm mid anterior subserosal, 2.7 cm left intramural, and 3.5 cm posterior subserosal fibroid. The patient had an uncomplicated procedure, blood loss of 250 cc with surgery completed in 110 minutes. Myomectomy included removal of a 9 cm fundal subserosal fibroid, 2 cm subserosal fibroid adjoined to the 9 cm fibroid, 3.5 cm posterior subserosal fibroid.
In the recovery room and 6 hours postoperatively, the patient had no subjective complaints with stable vitals. That evening, the patient reported incisional pain with slight erythema surrounding incision on superior aspect. On further physical examination, crackling consistent with crepitus was present across entire superior aspect of the incision, extending 2 cm superiorly. The patient noted to have tenderness during examination. Inferior to the incision, there was no pain on physical examination. No abdominal pain was noted on the upper quadrants of the abdomen. Subjectively, the patient denied nausea or vomiting, tolerating diet, and passing gas. The patient was promptly nothing by mouth (NPO) for possible surgery optimization, serial abdominal examinations, and CT was obtained immediately.
Computed tomography abdomen and pelvis demonstrated extensive subcutaneous emphysema along the anterior abdominal wall with mild surrounding fatty stranding (Figure 1). There was no evidence of fluid collection or abscess. The patient was subsequently receiving serial abdominal examinations, vitals remained stable, and repeat complete blood count demonstrated a stable hemoglobin, from 13.4 to 12.9 g/dL, and appropriate postoperative white blood cell count. The patient remained afebrile and symptoms began to resolve. She was discharged on postoperative day 2 with counseling for return precautions of signs or symptoms of infection or bleeding.
Discussion
Postoperative crepitus has a wide range of differential diagnosis. Differential diagnosis includes necrotizing fasciitis and perforated viscus and subcutaneous hematomas. Subcutaneous emphysema is a benign finding that is rare in open laparotomy cases and is more commonly seen in laparoscopic cases. This is secondary to multiple abdominal trocar entry attempts, improper cannula placement, loose fitting cannula/skin and fascial entry points, use of >5 cannulas, use of cannulas as fulcrums, torque of the laparoscope, increased intra-abdominal pressure, and procedures lasting >200 minutes. In this case, prompt awareness of patient’s incision pain, close monitoring of vitals, serial abdominal exams, imaging to identify any other occult findings are shown.
Subcutaneous emphysema is a rare finding after open abdominal surgery, but plausible. Likely mechanism included intra-abdominal air traversing through various planes of the abdomen from retroperitoneum to the subcutaneous layer. It is benign and self-resolving, as noted in two other identified case reports and in our case as well [1],[2].
Of note, a rare instance of a subcutaneous hematoma has been noted after subcutaneous emphysema in a reported case report by Khandelwal et al. [3]. While this report was in a mediastinal surgery, nonetheless, the subcutaneous tissue is a richly vascular layer. Given large free space in the subcutaneous layer, subcutaneous hematomas may arise as bleeding from the subcutaneous vessels could occur. Ultimately, the reported case of a subcutaneous hematoma following subcutaneous emphysema resolved within 10 days.
Conclusion
Crepitus is rarely seen in open/laparotomy cases. However, in the event of crepitus noted in postoperative physical examination, close monitoring and prompt action must occur. Morbid complications including necrotizing fasciitis and perforated viscus must be considered. This case report highlights the importance of high quality physical examination, early action to findings such as crepitus, and an appreciation of the abdominal/pelvic anatomy.
REFERENCES
1.
Xu C, Elkas JC, Hamilton CA. Benign, self-resolving subcutaneous emphysema and abdominal crepitus after open gynecologic surgery. Obstet Gynecol Cases Rev 2021;8(1):193. [CrossRef]

2.
Foote JR, Kohler MF, Young-Pierce J. Case report of massive subcutaneous emphysema: A benign postoperative finding. Obstet Gynecol Cases Rev 2014;1(2):012. [CrossRef]

3.
Khandelwal A, Kapoor I, Prabhakar H, Mahajan C. Subcutaneous hematoma following subcutaneous emphysema: An occult association. Indian J Crit Care Med 2017;21(9):618–9. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Richard Hsu - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
George Contos - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2023 Richard Hsu et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.