|
Case Report
Acute disseminated intravascular coagulation developed after suction and evacuation in an intrauterine fetal death: A case report
1 Department of Obstetrics and Gynecology, King Abdulaziz Medical City, National Guard Health Affairs, Riyadh, Saudi Arabia
Address correspondence to:
Wafa Alshahrani
Department of Obstetrics and Gynecology, King Abdulaziz Medical City, National Guard Health Affairs, Riyadh,
Saudi Arabia
Message to Corresponding Author
Article ID: 100216Z08WA2025
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Alshahrani W, Elsheikh M. Acute disseminated intravascular coagulation developed after suction and evacuation in an intrauterine fetal death: A case report. J Case Rep Images Obstet Gynecol 2025;11(2):38–41.ABSTRACT
Introduction: Disseminated intravascular coagulation (DIC) is defined as a hypercoagulable state leading to micro and macrovascular clotting compromising the blood flow leading to organ dysfunction. Most patient presenting with DIC will have a history of severe infection, recent trauma, hepatic failure, malignancy, or post-obstetrical bleeding. As the consequences of DIC can be fatal, it is crucial to be recognized as early as possible.
Case Report: We are presenting to you a case of intrauterine fetal death at 19 weeks complicated by DIC due to retained placenta leading to massive blood transfusion and intensive care unit (ICU) admission.
Conclusion: Disseminated intravascular coagulation is one of the complicated of massive uterine hemorrhage and early recognition in important for the patient’s mortality and morbidity.
Keywords: Blood transfusion, Disseminated intravascular coagulation (DIC), Intrauterine fetal death (IUFD), Obstetrical hemorrhage
Introduction
Complications post-surgical abortion, suction and evacuation, are rare ranging from 0.7–3% [1],[2],[3]. Possible complications during surgery include hemorrhage, infection, cervical laceration, and uterine perforation [4]. Massive hemorrhage post-abortion can lead to catastrophic complications including disseminated intravascular coagulation (DIC). The uncontrolled blood loss can lead to massive blood transfusion or in severe cases can lead to maternal mortality [5]. It was noted that suction and evacuation for fetal death was more linked to maternal mortality and morbidity compared to when it is done for termination of pregnancy [3]. Disseminated intravascular coagulation can be the consequence of massive hemorrhage or idiopathic [6]. It is believed that during the time of separation of the membrane and the placenta, platelet activation, thrombin generation, and release of granulation tissue factors occur leading to DIC [7]. The incidence of DIC was noted to be in case where the fetus was retained in the uterus for a period of time. In addition, it was noted that coagulopathy pathways were mediated by the thrombin like material produced from the retained product of conception [8]. There are a few studies discussing the association between fetal death and the development of DIC [3]. Herein, we are presenting a case of fetal death at 19 weeks which was complicated by DIC and ICU admission.
Case Report
A 39-year–old woman, Gravida 9, Para 5, with a history of two abortions, at 26 weeks of gestation by sure last menstrual period (LMP), who is not known to have any medical disease with her surgical history significant for previous five cesarean section, presented to the Emergency Department complaining of no fetal movements felt for days. Her bedside scan showed no fetal heart with spalding and floating ball signs noted. The patient was referred to the clinic for an official ultrasound to confirm the diagnosis. The scan showed a single fetus with negative cardiac activity and all fetal measurements were going with 19 weeks plus 5 days.
The patient was counseled regarding the findings and the need to start termination of pregnancy using Misoprostol as inpatient. She was given Misoprostol 200 mcg vaginal for a total of two doses 4 hours apart followed by 3 more doses 200 mcg sublingual 4 hours apart. She was shifted to labor and delivery as she was 5 cm dilated with regular strong contractions noted.
The patient progressed to full dilation smoothly with no augmentation needed. Non-viable fetus was delivered smoothly with no complications. Cord was clamped and cut. Oxytocin 10 units intramuscular (IM) and 20 units intravenous (IV) were started. Fetus was examined: Gender is a boy with fluid accumulation noted around the entire head. Skin maceration was noted. No other gross pathological findings were noted. Bedside scan was done showing part of the placenta near the cervix. Scar was intact.
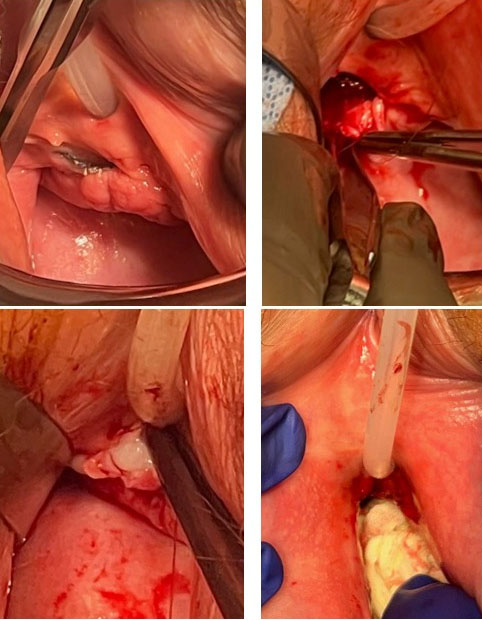
Suddenly, the patient started to bleed profoundly with blood pressure reaching 80 over 44. The decision was made and explained to the patient regarding the need to proceed with surgery for manual removal of the placenta and she agreed. The patient was pushed immediately to the operating table and was put under sedation in a Lithotomy position.
During the surgery, the patient had massive bleeding and blood transfusion began. Parts of the placenta were removed in pieces using manual removal, suction and evacuation. The patient was placed in a Trendelenburg position due to massive hypotension. Fresh frozen plasma was given as well. The patient received one dose of Cefazolin and Metronidazole intraoperatively. The patient’s blood was starting to become thinner and massive hemorrhage was begun, therefore, the suspicion of DIC was raised. Arterial blood gas (ABG) was showing Hgb level of 6.4 after receiving 2 units of packed red blood cells (PRBCs) with pH of 7.19 and CO2 of 32. The patient was intubated immediately by anesthesia and a Central line was inserted. Intensive care unit was contacted to book the patient for a bed due to massive bleeding with estimated blood loss of 4000 mL since delivery. Repeated ultrasound (US) showed clear endometrial line with minimal clots in the lower segment.
The patient has received a total of seven units of packed RBC, five units of fresh frozen plasma, four doses of Carboprost, one dose of Misoprostol, and one dose of Methergine IM intraoperatively. Vaginal packing was inserted at the end of the surgery. The patient was shifted to the ICU for monitoring. After arriving at the ICU, the patient was started on Inotropes to increase her blood pressure. Labs were taken which showed low levels of Fibrinogen to which 4 grams of Fibrinogen were given. The patient was given another unit of PRBC and 6 units of platelets. Labs showed normal Liver Function test and Creatinine level. The patient had adequate urine output. Her Hgb level increased to 99. Electrocardiogram (ECG) was done which was unremarkable.
The patient was extubated after being observed in the ICU for 24 hours. She received two more units of packed RBC. The patient’s labs and vital signs started to show great improvements. Vaginal pack was removed with no signs of active bleeding. Due to high levels of Troponin, Cardiology was contacted to which ECG and Cardiac Echocardiogram were carried out showing unremarkable results. The patient was shifted to the ward in stable condition. During the patient’s stay, she was kept of regular Carboprost IM every 6 hours and prophylactic antibiotics for 72 hours. The patient stayed a total of 6 days in the hospital post delivery. The patient was discharged in stable condition with a follow-up in the clinic for pathology results.
Discussion
Disseminated intravascular coagulation is a pathological disruption in the process of hemostasis which leads to activation of the coagulation cascade leading to deposition of fibrin. This will lead to activation of plasmin leading to fibrinolysis in addition to formation of microvascular thrombi. Eventually, multiorgan failure will occur due to depleted coagulation factors and platelets [9].
Affected women will tend to present with massive hemorrhage and symptoms of shock. Around 1–5% of patients affected with DIC are pregnant [10]. Disseminated intravascular coagulation leads to extreme maternal outcomes such as blood transfusion, hysterectomy, or death. As for the obstetric complications, patients with DIC are more likely to have postpartum hemorrhage, preeclampsia, placenta abruption, amniotic fluid embolism, and sepsis [11]. Obstetrical clinical manifestation ranges between severe uterine bleeding and bleeding from the intravenous sites or bladder catheter. As the bleeding increase, the patient will start to develop shock and becomes vitally unstable [12]. Laboratory workup tends to show thrombocytopenia, prolonged prothrombin time, and low fibrinogen levels [13]. Early recognition is the key in the diagnosis of DIC, especially if the patient presented with massive bleeding and in shock status. Management mainly focuses on the delivery or termination of pregnancy followed by supportive measurements including blood product transfusion such as packed red blood cells, platelets, and plasma.
Pelvic packing is considered a crucial step in the management of massive bleeding in patients who are hemodynamically unstable [14]. It was first described in 1926 by Logothetopulos as an intervention to decrease severe pelvic hemorrhaging [15]. The concept behind this approach is to create a physical tamponade in order to decrease the bleeding and allow more time for the uterotonic medications to reach their desired effect [14]. Patients who have vaginal packing should be monitored for any signs of deterioration and in case of any changes, a second look surgery should be carried out in 24–48 hours [15],[16].
The only effective treatment is the reversal of the underlying cause. Anticoagulants are rarely used. Platelets may be transfused if counts are less than 5000–10,000/mm and massive hemorrhage is occurring, and fresh frozen plasma may be administered to replenish coagulation factors and antithrombotic factors [9],[12].
Conclusion
In conclusion, the diagnosis of DIC is based on the clinical suspicion supported by the laboratory findings. Obstetrical cases that are complicated by massive bleeding are at risk of developing DIC. Patients who develop DIC require close observation in the ICU along with blood product transfusion to prevent further deuteriation. Early recognition is crucial to decrease maternal morbidity and mortality.
REFERENCES
1.
Gonzalez MG, Wei RM, Hatch KD, Gries LM, Hill MG. A novel treatment for massive hemorrhage after maternal trauma in pregnancy. AJP Rep 2019;9(1):e27–9. [CrossRef]
[Pubmed]

2.
Slofstra SH, Spek CA, ten Cate H. Disseminated intravascular coagulation. Hematol J 2003;4(5):295–302. [CrossRef]
[Pubmed]

3.
Ben-Ami I, Weizman NF, Schneider D, Pansky M, Halperin R. Coagulopathy associated with dilation and evacuation for second-trimester abortion. Acta Obstet Gynecol Scand 2012;91(1):10–15. [CrossRef]
[Pubmed]

4.
Frick AC, Drey EA, Diedrich JT, Steinauer JE. Effect of prior cesarean delivery on risk of second-trimester surgical abortion complications. Obstet Gynecol 2010;115(4):760–64. [CrossRef]
[Pubmed]

5.
Kerns J, Steinauer J. Management of postabortion hemorrhage: Release date November 2012 SFP Guideline #20131. Contraception 2013;87(3):331–42. [CrossRef]
[Pubmed]

6.
Erez O. Disseminated intravascular coagulation in pregnancy – Clinical phenotypes and diagnostic scores. Thromb Res 2017;151 Suppl 1:S56–60. [CrossRef]
[Pubmed]

7.
Erez O, Mastrolia SA, Thachil J. Disseminated intravascular coagulation in pregnancy: Insights in pathophysiology, diagnosis and management. Am J Obstet Gynecol 2015;213(4):452–63. [CrossRef]
[Pubmed]

8.
Letsky EA. Disseminated intravascular coagulation. Best Pract Res Clin Obstet Gynaecol 2001;15(4):623–44. [CrossRef]
[Pubmed]

9.
Levi M. Disseminated intravascular coagulation (DIC) in pregnancy and the peri-partum period. Thromb Res 2009;123 Suppl 2:S63–4. [CrossRef]
[Pubmed]

10.
11.
ACOG. Postpartum Hemorrhage. October 2017. [Available at: https://www.acog.org/clinical/clinical-guidance/practice-bulletin/articles/2017/10/postpartum-hemorrhage]

12.
Belfort MA. Disseminated intravascular coagulation during pregnancy. UpToDate. 2022. [Available at: https://teksmedik.com/uptodate20/d/topic.htm?path=disseminated-intravascular-coagulationduring-pregnancy]

13.
Guha P. Disseminated intravascular coagulopathy following induced second trimester curettage abortion. ISRN Obstet Gynecol 2011;2011:591760. [CrossRef]
[Pubmed]

14.
Battaloglu E, Cooper J. Emergency management of pelvic trauma. Orthopaedics and Trauma 2022;36(2):53–60. [CrossRef]

15.
Li Q, Dong J, Yang Y, Wang G, Wang Y, Liu P, et al. Retroperitoneal packing or angioembolization for haemorrhage control of pelvic fractures—Quasi-randomized clinical trial of 56 haemodynamically unstable patients with Injury Severity Score ?33. Injury 2016;47(2):395–401. [CrossRef]
[Pubmed]

16.
Yoong W, Lavina A, Ali A, Sivashanmugarajan V, Govind A, McMonagle M. Abdomino-pelvic packing revisited: An often forgotten technique for managing intractable venous obstetric haemorrhage. Aust N Z J Obstet Gynaecol 2019;59(2):201–7. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Wafa Alshahrani - Acquisition of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Mohammed Elsheikh - Conception of the work, Design of the work, Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2025 Wafa Alshahrani et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.